
Bioreactance-based passive leg raising test can predict fluid responsiveness in elderly patients with septic shock
Introduction
Fluid management is of critical importance and challenging during the treatment of patients with septic shock. Positive fluid therapy could effectively improve the hemodynamic stability, decrease the complication and mortality of patients (1). However, this approach is not always benefit to patients, it is associated with many risks, such as acute heart failure and acute pulmonary edema especially for elderly patients. Thus, accurately predicting fluid responsiveness (FR) and thus to estimate whether the patient will benefit from fluid therapy seems particularly important. Recent studies have demonstrated that one simple effective method for predicting FR is passive leg raising (PLR) test (2). Researchers could estimate whether the patient is fluid responsive through monitoring the hemodynamic changes before and after PLR. This study intends to predict FR of elderly patients with septic shock using bioreactance-based noninvasive cardiac output monitoring (NICOM) PLR test, to evaluate the value of this approach and compare to the central venous pressure (CVP) for predicting FR.
Methods
Patients
Patients over 60 years old with septic shock were enrolled from the Department of Critical Care Medicine of Zhejiang Hospital, Hangzhou, China, from October 2012 to October 2015. Diagnostic criteria for sepsis were as per the American College of Chest Physicians (ACCP) and the Society of Critical Care Medicine (SCCM), on the basis of infection occurring accompanied by at least two of the following: (I) body temperature ﹥38.3 or <36 °C; (II) heart rate (HR) ﹥90 beats/min; (III) respiratory ﹥20 beats/min or PaCO2 <32 mmHg; (IV) white blood cell (WBC) count ﹥12×109/L or <4×109/L or normal WBC count with greater than 10% immature forms. Septic shock was defined as sepsis-induced hypotension. The inclusion criteria were one or more of the following signs of tissue hypoperfusion: (I) systolic blood pressure <90 mmHg or decreased more than 40 mmHg compared to baseline level; (II) hourly urine output <0.5 mL/kg for more than 2 h; (III) HR ﹥100 beats/min; (IV) skin mottling. The exclusion criteria were as follows: (I) less than 60 years; (II) intra-abdominal hypertension (intra-abdominal pressure ﹥16 mmHg) (3); (III) organic heart disease (such as: mitral valve stenosis or intracardial shunt); (IV) intracranial hemorrhage or potential intracranial hemorrhage; (V) NICOM signal instability; (VI) other types of shock. This study was approved by the Ethics Committee of Zhejiang Hospital.
Measurements
Two dual-electrode stickers were placed on the right side of the chest wall, while another two stickers were placed on the left and connected to the NICOM system (Cheetah Medical, USA) for continuous recording of the following hemodynamic parameters: CO, HR, and noninvasive blood pressure (NIBP). Subclavian or jugular vein catheters (Arrow, USA) were put in place and connected to the monitor (Philips Healthcare, MP20, Germany) to record CVP.
Protocol
Patients enrolled in this study were managed with the following protocol. Baseline 1: patients were placed in a semi-recumbent position with the head of the bed elevated to 45° and the foot of the bed remaining horizontal; PLR: patients were placed in a supine position with their lower limbs elevated to 45°; baseline 2: patients were in a semi-recumbent position again, the same as in baseline 1; volume expansion (VE): 250 mL of normal saline solution was infused through the vein catheters within approximately 10 min. The NICOM system was used to record hemodynamics minute by minute during the 26 min or more, including: (I) 3 min of baseline 1; (II) 3 min of PLR; (III) 10 min of baseline 2; (IV) 10 min or more of VE (Figure 1). Throughout the protocol the ventilator parameters and the dosage of the vasoactive agents remained unchanged. Patients whose cardiac output (CO) increased by ≥10% were defined as responders, while those whose CO increased by <10% were defined as non-responders. This study was approved by the Ethics Committee of Zhejiang Hospital, with all the patients and their families have signed informed consent forms before participating in the study.
Statistics
Data were expressed as mean and standard deviation (SD). PLR induced change in CO was calculated as follows: ΔCOPLR% = [(CO after PLR) − (CO before PLR)] ×100/ (CO before PLR). VE induced change in CO was calculated as follows: ΔCOVE% = [(CO after VE) − (CO before VE)] ×100/(CO before VE). Comparisons of hemodynamic variables before and after intervention were made using paired t-test, and the comparisons between responders and non-responders were conducted using a two-sample t-test. The Pearson correlation coefficient was used to measure the linear correlations between ΔCOPLR% and ΔCOVE%, and between CVP and ΔCOVE%. All statistical tests were performed using SPSS (version 21.0, IBM, NY, USA), with P<0.05 being considered statistically significant.
Results
Demographic data of the 50 patients tested is presented in Table 1. Nearly half of the patients were treated with vasoactive agents. There were no significant differences in heights, weights, ages, body surface areas (BSA), and dosages of norepinephrine and dopamine between the two groups (P﹥0.05).
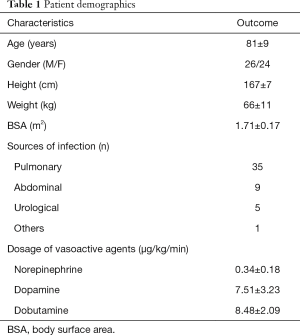
Full table
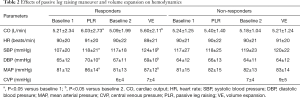
Effects of PLR and VE on hemodynamics
Among the 50 patients, 26 were responders and 24 were non-responders. In responders, compare to their baseline CO increased obviously after PLR and VE (P<0.05), while in non- responders compare to their baseline CO didn’t increase obviously (P﹥0.05). In responders and non- responders, the changes in HR before and after PLR and VE were not statistically significant (P﹥0.05) (Table 2).
Full table
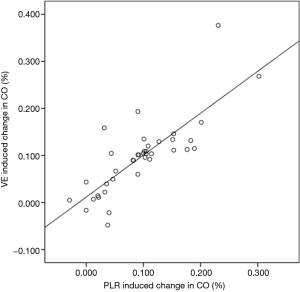
Analysis of correlation coefficient values
There was a good correlation between PLR induced change in CO (ΔCOPLR) and VE induced change in CO (ΔCOVE) [r=0.80 (0.64–0.90)] (Figure 2), and there was no correlation between VE induced change in CO (ΔCOVE) and CVP [r=0.12 (−0.16–0.32)].
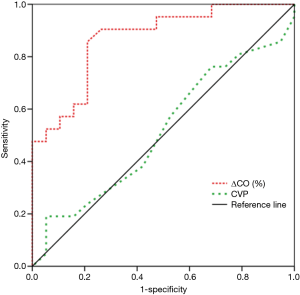
Values of ΔCOVE and CVP for predicting FR
The area under the ROC curve of CVP and PLR induced changes in CO (ΔCOPLR) for predicting FR was 0.477 and 0.883 respectively. The ΔCOPLR ≥10% was found to predict FR with a sensitivity of 86% and specificity of 79% (Figure 3).
Discussion
Our study showed that bioreactance-based PLR test is a simple and accurate method to predict FR in elderly patients with septic shock and CVP is hardly have the demanded accuracy for predicting FR. The percentage of CO response to PLR correlated very closely to the change of CO induced by fluid infusion test while the CVP didn’t. Our finding is in accordance with Benomar’s study that it is valid to use the bioreactance-based NICOM system to predict FR from changes in CO during PLR with patients after cardiac surgery (4). And Marik’s study enrolled 34 hemodynamic unstable ICU patients (5), indicating that bioreactance-based PLR test is accuracy enough for predicting FR in a large amount of patients.
Fluid therapy is a usual approach in the management of hemodynamic unstable ICU patients, whether for patients with septic shock or any other patients, positive fluid therapy could increase CO and thus to improve the tissue perfusion prognosis and to decrease the mortality of patients. However, inappropriate fluid therapy will cause many complications and thus bring about undesirable outcomes. Consequently, during the past decades countless efforts have been made to accurately predicting FR, from the static indicators to predictors based on heart-lung interactions such as SVV and PPV, but all have some limitations (6,7).
Recent researches have shown that a simple safe method is PLR test. By elevating the lower limbs to 45°, inducing passive transfer of blood contained in the venous compartment of the lower limbs and of the abdominal compartments to the heart, it thus can increase about 300 mL cardiac preload of the heart (2,8). A large number of studies (9-11) have designed to test its reliability for predicting FR and a meta-analysis (12) have confirmed its diagnostic accuracy. PLR serve as a “self-volume challenge”, it is simple, reliable and safe, since the influence of PLR to cardiac preload will disappear immediately when the elevated limbs are horizontal again (8).
Although PLR is an effective way for predicting FR, it must perform under the guidance of technologies such as pulse index continuous CO (PICCO) (11) and echocardiography (9). Therefore, predicting FR based on CVP is widely used in critical care setting for its convenience and low costs. However, our study showed that there was a very low correlation between the change of CO after giving fluid bolus and CVP at baseline 2 suggesting that CVP is not useful in predicting FR. It is also confirmed by a meta-analysis in recent years which included ten studies that the correlation coefficient between CVP and change in stroke index/cardiac index was poor (r=0.18) (13). CVP represents the pressure of right atrium and near superior and inferior vena cava, can not reflect the true blood volume. Moreover, the measurement of CVP is greatly influenced by artificial factors such as the proficiency of operator and the position of the sensor. Maybe it can partly explain the reason why CVP performs so badly in predicting FR.
For the past years, physicians devoted to develop more efficient devices for hemodynamic monitoring. There is no doubt that the most ideal device should be accurate noninvasive easy to use and cheap. NICOM is such a new device for noninvasive hemodynamic measuring. It is based on an analysis of relative phase shifts of an oscillating current that occur when this current traverses the thoracic cavity to calculate the hemodynamic parameters and just need four double-electrode stickers placed on the chest wall (14). Comparing with the thermodilution which serves as the “gold standard” of hemodynamic measurements, its accuracy has already been demonstrated in the previous studies (15,16). In addition, it has a shorter response time for hemodynamic challenges (17) which is emphasized in the daily work. Clinical determination of giving a fluid bolus is depend on whether the patient will benefit from it, thus a method that is accuracy, easy to get, efficient is preferable, for predicting FR. Considering this there is no doubt that bioreactance-based PLR test can be routinely used to predict FR, since the assessment could be finished in 6 min.
In a recent study, Kupersztych-Hagege and his colleagues found that the correlation between the changes in pulse contour analysis-derived CI and NICOM derived CI induced by VE is very poor (18), demonstrating that bioreactance-based PLR test may fail to predict FR. The reasons may be as follows, first, the degree of bioimpedance unreliability was related to the extent of lung injury and fluid accumulation within the thorax (19), and maybe so is the bioreactance VE would reduce haemoglobin levels and possibly alter the bioreactance readings. In this study, although all the participants were patients with septic shock, there was no occurrence of acute respiratory distress syndrome and pulmonary edema in these 80 patients, what’s more we only used half of the fluid, maybe it is the main difference between the two studies. Although we found a relatively ideal result, we believe that any new device will confront many problems during the progress of clinical popularization. These were the very aspects that the following study should focus more on.
In this study, we used 250 mL normal saline, instead of the commonly used 500 mL (9-11), to perform a volume challenge. Firstly, because clinical use of fluid to perform a fluid infusion test is 250 mL normal saline; secondly, only about 50% of critically ill patients were fluid responders (8), the patients enrolled in this study were mostly the elders, these patients have a decreased number of myocardial cells and hyperplasia of collagen tissues, thus having a higher risk of heart failure, using this volume of fluid is to reduce the detrimental effects.
Our study had some limitations. First, all the patients were septic shock. Therefore, it is not known whether or not our results can be extrapolated to other populations for whom fluid optimization is necessary for treatment. Second, we excluded patients with organic heart disease for fearing that it will in some extent influence the prediction of FR referring to Renner’s study (20) without test it.
In conclusion, in the specific population of elderly patients we studied here, bioreactance-based PLR test but not CVP could accurately predict FR of elderly patients with septic shock. Because of its practicability and effectiveness, this approach deserves a further promotion in daily practice.
Acknowledgements
The authors are grateful to Prof. Jean-Louis Teboul for his help in conception.
Funding: This work was funded by the Zhejiang Medical and Health Science and Technology Project (NO. 2013KYB004, 2013ZDA001, 2017ZD001); the Zhejiang Traditional Chinese Medicine Research Project (No. 2011ZZ001).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Ethics Committee of Zhejiang Hospital (approval number: 2013-28). All the patients and their families have signed informed consent forms before participating in the study.
References
- Phan TD, Ismail H, Heriot AG, et al. Improving perioperative outcomes: fluid optimization with the esophageal Doppler monitor, a metaanalysis and review. J Am Coll Surg 2008;207:935-41. [Crossref] [PubMed]
- De Backer D. Can passive leg raising be used to guide fluid administration? Crit Care 2006;10:170. [Crossref] [PubMed]
- Mahjoub Y, Touzeau J, Airapetian N, et al. The passive leg-raising maneuver cannot accurately predict fluid responsiveness in patients with intra-abdominal hypertension. Crit Care Med 2010;38:1824-9. [Crossref] [PubMed]
- Benomar B, Ouattara A, Estagnasie P, et al. Fluid responsiveness predicted by noninvasive bioreactance-based passive leg raise test. Intensive Care Med 2010;36:1875-81. [Crossref] [PubMed]
- Marik PE, Levitov A, Young A, et al. The use of bioreactance and carotid Doppler to determine volume responsiveness and blood flow redistribution following passive leg raising in hemodynamically unstable patients. Chest 2013;143:364-70. [Crossref] [PubMed]
- Pinsky MR. Functional haemodynamic monitoring. Curr Opin Crit Care 2014;20:288-93. [Crossref] [PubMed]
- Teboul JL, Monnet X. Pulse pressure variation and ARDS. Minerva Anestesiol 2013;79:398-407. [PubMed]
- Monnet X, Teboul JL. Volume responsiveness. Curr Opin Crit Care 2007;13:549-53. [Crossref] [PubMed]
- Préau S, Saulnier F, Dewavrin F, et al. Passive leg raising is predictive of fluid responsiveness in spontaneously breathing patients with severe sepsis or acute pancreatitis. Crit Care Med 2010;38:819-25. [Crossref] [PubMed]
- Monnet X, Rienzo M, Osman D, et al. Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med 2006;34:1402-7. [Crossref] [PubMed]
- Monnet X, Bataille A, Magalhaes E, et al. End-tidal Carbon dioxide is better than arterial pressure for predicting volume responsiveness by the passive leg raising test. Intensive Care Med 2013;39:93-100. [Crossref] [PubMed]
- Cavallaro F, Sandroni C, Marano C, et al. Diagnostic accuracy of passive leg raising for prediction of fluid responsiveness in adults: systematic review and meta-analysis of clinical studies. Intensive Care Med 2010;36:1475-83. [Crossref] [PubMed]
- Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest 2008;134:172-8. [Crossref] [PubMed]
- Keren H, Burkhoff D, Squara P. Evaluation of a noninvasive continuous cardiac output monitoring system based on thoracic bioreactance. Am J Physiol Heart Circ Physiol 2007;293:H583-9. [Crossref] [PubMed]
- Squara P, Denjean D, Estagnasie P, et al. Noninvasive cardiac output monitoring (NICOM): a clinical validation. Intensive Care Med 2007;33:1191-4. [Crossref] [PubMed]
- Raval NY, Squara P, Cleman M, et al. Multicenter evaluation of noninvasive cardiac output measurement by bioreactance technique. J Clin Monit Comput 2008;22:113-9. [Crossref] [PubMed]
- Squara P, Cecconi M, Rhodes A, et al. Tracking changes in cardiac output: methodological considerations for the validation of monitoring devices. Intensive Care Med 2009;35:1801-8. [Crossref] [PubMed]
- Kupersztych-Hagege E, Teboul JL, Artigas A, et al. Bioreactance is not reliable for estimating cardiac output and the effects of passive leg raising in critically ill patients. Br J Anaesth 2013;111:961-6. [Crossref] [PubMed]
- Critchley LA, Calcroft RM, Tan PY, et al. The effect of lung injury and excessive lung fluid, on impedance cardiac output measurements, in the critically ill. Intensive Care Med 2000;26:679-85. [Crossref] [PubMed]
- Renner J, Broch O, Duetschke P, et al. Prediction of fluid responsiveness in infants and neonates undergoing congenital heart surgery. Br J Anaesth 2012;108:108-15. [Crossref] [PubMed]
Cite this article as: Hu C, Cai G, Yan J, Tong H, Lv X, Xu Q, Chen S, Zhang H. Bioreactance-based passive leg raising test can predict fluid responsiveness in elderly patients with septic shock. J Emerg Crit Care Med 2017;1:7.



