
Opportunities and challenges in the emergency and critical care medicine
Emergency and critical care medicine is one of the most challenging areas in medicine, which not only has become increasingly complex, involving joint efforts of the whole hospital, even multidepartment and multi-system cooperation from society, but also requires continuously updated medical technology and concepts. In addition, with the rapid economic development and aging of the population, expectations from society for better diagnosis and treatment of emergency and critical illness are on the rise. However, due to historical reasons, China and even rest of the Asia have been following the pace of America and European countries in emergency and critical care medicine. Hence the need for establishing a society and writing clinical guidelines of this area for Asia has become much greater. Therefore, we work together, striving for setting up the Asia Society of Emergency and Critical Care Medicine (ASECCM) and holding the First Asia Summit on Emergency and Critical Care Medicine to share experience and achievements, explore suitable treatment modes for Asian patients and write Asia clinical guidelines in emergency and critical care medicine. We’ve invited well-known experts from China, Japan, Korea, Singapore, Taiwan, Hong Kong, India and other countries and areas to join the ASECCM.
A special feature of the summit is that the keynote speakers have prepared their topic into review articles that will be published in the Journal of Emergency and Critical Care Medicine. These review articles include most updated information in the treatment of critical illness. Management of community pneumonia in the emergency department is challenging for clinicians and required multidisciplinary team. Lim and colleagues discussed the importance of Prompt recognition of severe CAP and timely, appropriate initiation of antimicrobials and execution of resuscitation bundles in the emergency department (ED) (1). Fever is a common phenomenon in the intensive care unit (ICU) and its management has been widely debated. On one hand, fever is a natural response to the inflammatory stimulus and fever will help to eradicate pathogens. However, fever also increases energy expenditure in critically ill patients. Thus, the use of antipyretic therapy is controversial (2,3). Egi and colleagues discussed several important issues in the management of fever for critically ill patients by systematically reviewing literature. They concluded that “if there is decompensation of vital signs including tachycardia, tachypnea or patient suffering caused by fever, antipyretics should be used to prevent derangement.” (4). Anticoagulation is important for the management of extracorporeal membrane oxygenation (ECMO) to keep the circuit patent. In this focused issue, Wong and colleagues discussed several anticoagulation strategies in the ECMO running and they proposed bleeding bundles to control bleeding since massive hemorrhage may be life threatening in patients with ECMO (5). Critical care ultrasound is becoming more and more important in the management of critical care and emergency patients (6,7). Some life-threatening conditions such as pneumothorax (8,9), intraabdominal hemorrhage, solid organ rupture and volume status can be readily identified by using bedside ultrasound (10). Hussain presented some key advances in critical care ultrasound in the summit. He focused on the sepsis and heart from an echocardiographic perspective (11). The full list of articles is shown in Table 1.
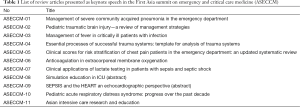
Full table
Furthermore, the summit publishes several consensus and guidelines including the management of chest pain, the use of ultrasound in the venous catheterization, trauma team and mechanical ventilation. These consensuses were developed with the most updated evidence and fully incorporated situations in Asia countries.
Acknowledgements
None.
References
- Lim TK, Chew MY. Management of severe community acquired pneumonia in the emergency department. J Emerg Crit Care Med 2018;2:2. [Crossref]
- Zhang Z. Antipyretic therapy in critically ill patients with established sepsis: a trial sequential analysis. PLoS One 2015;10:e0117279. [Crossref] [PubMed]
- Zhang Z, Chen L, Ni H. Antipyretic therapy in critically ill patients with sepsis: an interaction with body temperature. PLoS One 2015;10:e0121919. [Crossref] [PubMed]
- Egi M, Makino S, Mizobuchi S. Management of fever in critically ill patients with infection. J Emerg Crit Care Med 2018;2:10. [Crossref]
- Wong JJ, Lam JC, Mok YH, et al. Anticoagulation in extracorporeal membrane oxygenation. J Emerg Crit Care Med 2018;2:12. [Crossref]
- Zhang Z. Echocardiography for patients undergoing extracorporeal cardiopulmonary resuscitation: a primer for intensive care physicians. J Intensive Care 2017;5:15. [Crossref] [PubMed]
- Zhang Z, Chen L, Chen K, et al. The prognostic value of cardiac dysfunction assessed by bedside echocardiography in critically ill patients with COPD requiring mechanical ventilation: a study protocol. BMJ Open 2014;4:e005359. [Crossref] [PubMed]
- Chen L, Zhang Z. Bedside ultrasonography for diagnosis of pneumothorax. Quant Imaging Med Surg 2015;5:618-23. [PubMed]
- Zhang Z. Double lung point in an 18-month-old child: a case report and literature review. J Thorac Dis 2015;7:E50-3. [PubMed]
- Zhang Z, Hong Y, Liu N, et al. Diagnostic accuracy of contrast enhanced ultrasound in patients with blunt abdominal trauma presenting to the emergency department: a systematic review and meta-analysis. Sci Rep 2017;7:4446. [Crossref] [PubMed]
- Hussain A. AB001. Sepsis and the heart: an echocardiographic perspective. J Emerg Crit Care Med 2018;2:11. [Crossref]
Cite this article as: Hong Y. Opportunities and challenges in the emergency and critical care medicine. J Emerg Crit Care Med 2018;2:23.


