
ATLS and Trauma Team Training in the Netherlands
Introduction
In 1976 Dr. Jim Styner crashed his General Aviation aircraft in the plains of Nebraska. Because the treatment he and his family received in a small hospital “could be improved upon” he later developed a systematic approach for treating victims “during the first hour post-trauma”; a for-the-time very modern educational format was developed in parallel, resulting in what we now know as the advanced trauma life support (ATLS®) course (1).
Trialled in 1978 in Lincoln, Nebraska, the concept was adopted by the American College of Surgeons (ACS) and promulgated internationally in 1980.
The rest is history: ATLS® has become the standard in 66 countries (and counting); the ABCDE approach is widely accepted not only for trauma, but for acute medical and neurological conditions as well; derivates have been developed for use outside the hospital, in normal and austere circumstances; the military uses its own version.
A success story; or is it?
From early on there’s also been criticism; both from instructors and from students.
Criticism is important information; it should be listened to very carefully.
Below we describe how ATLS was introduced in the Netherlands; how feed-back was and is collected and how criticism is being reacted to.
ATLS and the Netherlands
When ATLS was introduced in 1995 the 2-day format was chosen for logistical and financial reasons. The Netherlands being a small country (area 16.5 K square miles, pop. 17 M) all courses were and are held in one training centre.
Very quickly the ATLS course became compulsory for residents in Surgery and Anaesthesia; over the last 10 years more and more Hospitals require all junior doctors to be ATLS certified. Because of the latter many students nowadays are very inexperienced when they come on the course. At present some 800 doctors are trained annually.
Criticism
Even though ATLS® has become the standard for trauma care in many countries several authors have their doubts (2-6). Some are for several reasons not in favour (7,8), and alternative courses have been developed (9).
It is interesting to note that in reviews no prospective trials were found assessing outcome of trauma care (10,11); better outcomes have also been reported (12-16).
In the Netherlands, as elsewhere, each course is evaluated by both instructors and students, using the form from the Faculty Manual.
During many years recurring criticisms regarding the course format were: “too many lectures with too little new information when compared to the Manual”; “too little opportunity to practise”; “unrealistic training”.
Comments like these have not been confined to the Netherlands. Several authors (17-20) report comparable opinions: students prefer problem-based learning over classical lectures.
A new format
Over the years several ATLS-based formats have been developed such as the American College of Surgeons (ACS) Trauma Evaluation and Management (TEAM) course that is aimed at medical students (21) but can also be used for educating in low and middle-income countries (22); the Primary Trauma course (16) is used for the same purpose. None of these however, would provide a solution to the first two criticisms mentioned above.
Therefore, Dutch ATLS decided in 2006 to devise a new format, at first only as an intellectual exercise. Since 2006 all “Dutch developments” have been reported during the annual ACS/International ATLS and ATLS Europe meetings.
Knowing that simulation is a very effective way for transferring knowledge and skills (23,24) that is also much liked by students, Dutch ATLS increased in its new format the number of moulage assessments, retaining only a few lectures.
The skills were rearranged in four blocks (A, B, C and D), each consisting of a plenary demonstration and plenary minilecture, followed by a scenario-based practical in small groups, dealing with all relevant psychomotor skills.
Although the program had been devised as a reaction to complaints by provider students, Dutch ATLS decided to run it, starting in 2007, at first as a trial with refresher candidates; to see whether it was viable and also because many versions of the refresher program that had been tried over the years had not been really satisfactory.
The program was very well received and with some minor modifications it has been used for the Refresher course till 2016. Dutch ATLS is of course very much aware of the fact that even after effective skills teaching, the student needs further practice in order to become proficient (25,26).
The candidates have been asked in their feed-back form whether they thought a comparable program could be used for the Provider course. A majority was of the opinion that provider candidates would need additional coaching because of their inexperience. The question then for Dutch ATLS was how to provide that coaching.
The ACS had announced in 2011 that an e-learning program was under construction and Dutch ATLS opted to wait for its completion, hoping it could be used for giving that extra coaching. The first version of the ACS program that was presented a year later obviously needed improvement.
As little information on that process became available, Dutch ATLS decided in 2014 to develop an e-learning program of its own.
E-learning
The ATLS Manual is very well “constructed” but the system behind that construction is not always easy to understand for a less experienced reader. For that reason, the Dutch e-learning program strives to translate knowledge from the Manual into a system that can be applied in practice; it takes the student, “by the hand”, through the different steps of assessing a trauma victim. In addition, it provides steps 1 and 2 of the 4-step method for teaching psychomotor skills; it teaches how to look at X-rays systematically and it also has a large number of self-assessment questions.
Finally, the student must successfully complete a newly developed MCQ test, before the 2-day face-to-face course can be attended. Extensive feed-back on that MCQ test is immediately provided to the student.
The e-learning program was finalized in June 2015; to follow it completely takes on average 10–12 hours.
A new Provider course
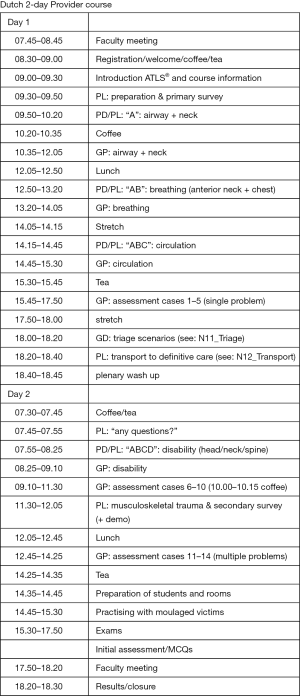
In order to make e-learning and a new face-to-face program fully complementary, Dutch ATLS then took the earlier mentioned refresher program and adapted it as required. Both were beta-tested 12 times from June to November 2015 and then introduced in its final version in January 2016. Figure 1 shows the present 2-day face-to-face program.
During the beta-testing period Dutch ATLS found that results (pass-rate and number of practical re-exams) had improved, but only slightly (unpublished data).
When the nearly completed 10th edition of ATLS was presented in June 2017 it was pleasant surprise to see that Dutch ATLS and the American College of Surgeons had been working along the same lines.
When using the refresher format in an adapted version for the new provider program Dutch ATLS had recognized from the start that the Refresher course would need a new program as well.
“Train the Team” training
ATLS® trains its students for performing as an individual (together with an “non-obstructive nurse”) but in real life in trauma care physicians and nurses work as a team. Understandably therefore, the third criticism mentioned above is that ATLS® training is unrealistic.
Apart from the fact that individual training is quite effective for “instilling the basics”, Dutch ATLS was very much aware that in the Netherlands physicians and nurses were being trained separately (ATLS® and TNCC® respectively) for taking care of trauma victims. Up to 2010 several schemes had been tried to train physicians and nurses together. To mention a few: having the lectures with a “mixed audience” but teaching specific skills and performing test initial assessments separately; having ATLS® and TNCC® courses at the same time but separately and organizing a half-day of training together; combining ATLS® and TNCC® and having a course “for all denominations”.
None of these experiments worked out well. Moreover, it became clear that a chance group of participants isn’t ideal for team training: to work as a team much depends on “knowing each other” and on the mutual trust that may develop over time. Clearly, to train for working as a team should also be done with the people who are part of such a team, in surroundings they are familiar with. In other words: team training should be done on-site and not in a training centre with a chance group of people (mark).
In 2009 Dutch ATLS and the Dutch Foundation for Trauma Nursing decided to develop a program for on-site training of hospital trauma teams. It was run for the first time in 2010.
That program was much indebted to a training scheme of the Netherlands Army Medical Services that had been in place since 2004.
That scheme recognizes that once basic skills are in place, learning is best achieved by doing, or in other words, that a higher level of proficiency is only reached by repeated experiences (27). Also, it takes into account that systematic feed-back by skilled observers enhances the learning experience, and finally it emphasizes that for efficient and effective team work excellent communication is a prerequisite (28-32).
In the Netherlands Army Medical Services this system has been and still is being used, in particular pre-deployment, for making people of varying backgrounds (junior doctors and military nurses with limited experience and medical orderlies with almost non-existent experience) work together in an effective and safe way.
A training session goes through the following phases: a team receives a message about a casualty being on the way. Then, in a simulated environment that is identical to where that team will be working later, all preparations are performed: assigning tasks, checking of equipment and medications, alerting additional personnel.
When the casualty, well-moulaged and well-prepared as to required behaviour, is brought in, the team listens to the hand-over, and then starts the assessment.
Following the c-ABCD approach the team, under a team-leader, does everything that is necessary, in real-time with real resources; either on the casualty or, for invasive procedures, on a manikin. Laboratory tests, X-rays and sonography are simulated but, again, in real-time.
Two instructors/case-managers serve as producers, guiding the scenario depending on the quality of care that is being delivered.
At the end of the assessment, the team leader, when necessary in consultation with medical specialists, decides when the casualty is ready to leave the emergency room, and after a hand-over the assessment phase is concluded. Immediately afterwards the emergency room (ER) is cleaned and consumables are replaced.
The next phase is the feed-back session, where the team itself goes through all steps of preparation and assessment; guided, when necessary, by the instructors. The Pendleton rules (“what went well; what could be improved upon”) are followed.
During the session 2 subjects are addressed: medical and communication/teamwork.
Ideally the team itself “discovers” medical shortcomings; in discussing communication and teamwork the instructors have a somewhat more guiding role. They steer the discussion in such a way that the team itself finds where improvements in those respects should be made.
Much attention is paid to the so-called “team conversation”: assessment should proceed in an orderly and pre-arranged fashion; all information should be shared; orders should be given by name and never “in the air”; orders should be repeated by the addressee who should report back on the result of that order; every team member is expected to speak up when necessary, but always in a timely and orderly fashion; thereby preventing confusion.
Training sessions as described above are repeated many times; every time with a different casualty (between 2004 and 2010, when the Netherlands were involved in Iraq and Afghanistan, a team had seen on average 120 different cases, before being deployed).
This format was changed for the civilian on-site training sessions because the session is a one-time affair and limited in duration. The instructors begin by visiting the Hospital in question to find out what the size and composition of its trauma team is; what its standard operating procedures (SOP) are, but also to find out what the Hospital expects from the training session. They then develop a scenario that is adapted to the situation in that particular Hospital. For example, if a hospital has no neurosurgeon practicing would include how to stabilize and transport a neurotrauma patient.
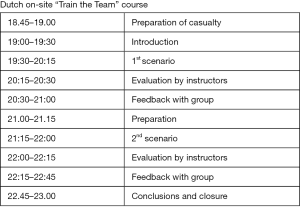
On the training day itself a program usually involving 2 cases is run, with 1 team performing and another observing (ideally via a video link). The observing team will perform on the next run, and the performers become the observers (Figure 2).

The program consists of simulated trauma team activations: a scenario call from ambulance dispatch is sent to the emergency department, after which the local SOP activating the trauma team is followed.
Once the team has arrived in the ER and has completed its preparations, the casualty is wheeled into the Trauma Room and after the hand-over assessment is begun. One instructor acts as case manager; the other assesses the processes, using a Crew Resource Management (CRM) checklist (Figure 3).
The team itself decides when to transfer the patient out of the Trauma Room, thereby ending the simulation; after which a de-briefing session is held. Group interaction and (if necessary) medical performance are carefully scrutinized; with comments from not only the instructors but also from the observing team.
This program, which has similarities to the ACS Rural Trauma Team Development course, has been well received and over the years many Hospitals have developed comparable programs of their own.
A new Refresher course
In parallel with the new Provider course Dutch ATLS developed a new refresher course, which was introduced in March 2016.
Based on previous experiences it was recognised that such a program on the one hand should inform the participants, who have at least 4–5 years’ experience in the field, on “What’s new in ATLS” and on the other be attractive by introducing something new.
After much deliberation the following format was agreed upon: the participants begin by reading the most recent edition of the ATLS® Manual and by completing the e-learning program (thereby getting an idea of “What’s new in ATLS”).
Then they come to a 1-day face-to-face program which begins with an overview of the developments in ATLS®, followed by five classic moulages and a written test (again, the “What’s new in ATLS” part). That part is followed by an introduction to CRM, which is then practised during ten “CRM moulages” (Figure 4).

For each of the “CRM moulages” a trauma team is constituted, consisting of a team leader, an “A” physician and a “BC” physician. A 4th student serves as the scribe; the 5th is the casualty. One instructor is the case manager, the other the CRM assessor. Both serve as nurses, when required. Students rotate through the different positions.
Alternatively a manikin is used as the casualty; in that case the 5th student observes.
Having five students in each group has no specific educational consideration (33).
Figure 5 shows the roster for the rotations.
Much attention is paid to the de-briefing session which mainly deals with CRM aspects. Feed-back is provided by the scribe (medical aspects) and the instructors (CRM aspects).
The program was generally speaking well accepted, although several instructors needed some time to get used to it. The fact that for practical reasons the program had to be introduced without a formal instructors’ day will have been of influence there.
As of June 2016, hospitals where several/many physicians are up for recertification can request to have the Refresher course on-site. This option has turned out to be highly successful and appreciated. In the future ATLS NL hopes to run the majority of Refresher courses that way; the contents will undoubtedly be further refined.
Results and feed back
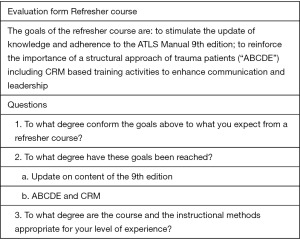
Every Refresher course is assessed afterwards, both by the students and the faculty. Figure 6 shows the student evaluation form; we use a 5-point Likert scale and an opportunity for open comments.
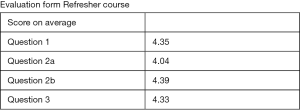
From its introduction in March 2016 up to July 2017 we’ve run 26 Refresher courses 520 participants; 432 of whom (83%) provided a useable form. The main results are shown in Figure 7.
From the open comments the following deserve mention: participants would like to have written information on the differences between the current edition of the ATLS® Manual and previous ones. Likewise, as CRM principles are not known to all participants more information on the subject before the course is requested. In general, on-site training is highly appreciated, although there are no differences in scoring results between participants who’ve been trained on-site and those who attended the course in the central training center.
Summary
At this moment ATLS NL is running a self-developed hybrid Provider course with e-learning and a face-to-face program with ample opportunity for practising the Initial Assessment.
Trauma Team and CRM training require basic ATLS knowledge and skills on the part of the students.
At present in the Netherlands Trauma Team and CRM training aren’t part of the ATLS Provider course; they are an essential part of the Dutch ATLS Refresher course and of the on-site “Train the Team” training course.
All on-site activities are highly appreciated; both team training for physicians and nurses, and Refresher courses for physicians only.
Acknowledgements
The author would like to thank Dr. James D. Gregory, FACS for his advice.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Atls Student Manual 9th (ninth) Edition. American College of Surgeons, Chicago, 2012.
- Davis M. Should there be a UK based advanced trauma course? Emerg Med J 2005;22:5-6. [Crossref] [PubMed]
- Nolan JP. Advanced trauma life support in the United Kingdom: time to move Emerg Med J 2005;22:3-4. [Crossref] [PubMed]
- McKeown D. Should the UK develop and run its own advanced trauma course? Emerg Med J 2005;22:6-7. [Crossref] [PubMed]
- Sarkar S, Worms R, Hall AP. Trauma training in the UK: is ATLS past its 'sell-by date'? Anaesthesia 2007;62:537. [Crossref] [PubMed]
- Wiles MD. ATLS: Archaic Trauma Life Support? Anaesthesia 2015;70:893-7. [Crossref] [PubMed]
- Thies KC, Scheffer GJ. Do we a need a European approach to trauma care? Resuscitation 2004;60:113-4. [Crossref] [PubMed]
- Thies KC, Nagele P. Advanced Trauma Life Support--a standard of care for Germany? No substantial improvement of care can be expected. Anaesthesist 2007;56:1147-54. [Crossref] [PubMed]
- Thies K, Gwinnutt C, Driscoll P, et al. The European Trauma Course--from concept to course. Resuscitation 2007;74:135-41. [Crossref] [PubMed]
- Jayaraman S, Sethi D, Chinnock P. Advanced trauma life support training for hospital staff. Cochrane Database Syst Rev 2014;22:CD004173. [PubMed]
- Shakiba H, Dinesh S, Anne MK. Advanced trauma life support training for hospital staff. Cochrane Database Syst Rev 2004.CD004173. [PubMed]
- Petroze RT, Byiringiro JC, Ntakiyiruta G., et al. Can focused trauma education initiatives reduce mortality or improve resource utilization in a low-resource setting? World J Surg 2015;39:926-33. [Crossref] [PubMed]
- Wang P, Li NP, Gu YF, et al. Comparison of severe trauma care effect before and after advanced trauma life support training. Chin J Traumatol 2010;13:341-4. [PubMed]
- van Olden GD, Meeuwis JD, Bolhuis HW, et al. Clinical impact of advanced trauma life support. Am J Emerg Med 2004;22:522-5. [Crossref] [PubMed]
- Navarro S, Montmany S, Rebasa P, et al. Impact of ATLS training on preventable and potentially preventable deaths. World J Surg 2014;38:2273-8. [Crossref] [PubMed]
- Ologunde R, Le G, Turner G, et al. Do trauma courses change practice? A qualitative review of 20 courses in East, Central and Southern Africa. Injury 2017;48:2010-16. [Crossref] [PubMed]
- Campbell B, Heal J, Evans S, et al. What do trainees think about advanced trauma life support (ATLS)? Ann R Coll Surg Engl 2000;82:263-7. [PubMed]
- Muenzberg M, Paffrath T, Matthes G, et al. Does ATLS trauma training fit into Western countries: evaluation of the first 8 years of ATLS in Germany. Eur J Trauma Emerg Surg 2013;39:517-22. [Crossref] [PubMed]
- Luedi MM, Wölfl CC, Wieferich K, et al. Teaching Advanced Trauma Life Support (ATLS): A nationwide retrospective analysis of 8202 lessons taught in Germany. J Surg Educ 2017;74:161-6. [Crossref] [PubMed]
- Ibrahim NK, Banjar S, Al-Ghamdi A, et al. Medical students preference of problem-based learning or traditional lectures in King Abdulaziz University, Jeddah, Saudi Arabia. Ann Saudi Med 2014;34:128-33. [Crossref] [PubMed]
- Ali J. The Trauma Evaluation and Management (TEAM) teaching module: its role for senior medical students in Canada. Can J Surg 2003;46:99-102. [PubMed]
- Kurdin A, Caines A, Boone D, et al. TEAM: A Low-Cost Alternative to ATLS for Providing Trauma Care Teaching in Haiti. J Surg Educ 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Borggreve AS, Meijer JMR, Schreuder HWR, et al. Simulation-based trauma education for medical students: A review of literature. Med Teach 2017;39:631-8. [Crossref] [PubMed]
- Ali J, Al Ahmadi K, Williams JI, et al. The standardized live patient and mechanical patient models--their roles in trauma teaching. J Trauma 2009;66:98-102. [Crossref] [PubMed]
- Okuda Y, Bryson EO, DeMaria S Jr, et al. The utility of simulation in medical education: what is the evidence? Mt Sinai J Med 2009;76:330-43. [Crossref] [PubMed]
- Knudson MM, Khaw L, Bullard MK, et al. Trauma training in simulation: translating skills from SIM time to real time. J Trauma 2008;64:255-63. [Crossref] [PubMed]
- Haerkens MH. Human factors and team performance. Thesis, Catholic University Nijmegen, the Netherlands 2017.
- Capella J, Smith S, Philp A, et al. Teamwork training improves the clinical care of trauma patients. J Surg Educ 2010;67:439-43. [Crossref] [PubMed]
- Siriratsivawong K, Kang J, Riffenburgh R, et al. Immersion team training in a realistic environment improves team performance in trauma resuscitation. Surgery 2016;160:586-90. [Crossref] [PubMed]
- Roberts NK, Williams RG, Schwind CJ, et al. The impact of brief team communication, leadership and team behavior training on ad hoc team performance in trauma care settings. Am J Surg 2014;207:170-8. [Crossref] [PubMed]
- Ford K, Menchine M, Burner E, et al. Leadership and Teamwork in Trauma and Resuscitation. West J Emerg Med 2016;17:549-56. [Crossref] [PubMed]
- Walcher F, Scheller B, Heringer F, et al. TEAM®-G (Trauma Evaluation and Management Germany). Serves as a basis for an interdisciplinary training in the emergency room. Unfallchirurg 2013;116:602-9. [Crossref] [PubMed]
- Rezmer J, Begaz T, Treat R, et al. Impact of group size on the effectiveness of a resuscitation simulation curriculum for medical students. Teach Learn Med 2011;23:251-5. [Crossref] [PubMed]
Cite this article as: Henny W. ATLS and Trauma Team Training in the Netherlands. J Emerg Crit Care Med 2018;2:25.



