Is chest X-ray in supine position for central lines confirmation a gold standard or a fallacy?
The ‘tip’ confusion
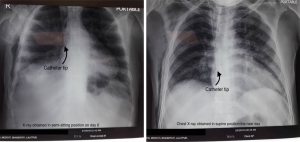
Central venous lines (CVL) are placed in settings like emergency departments, operation theaters and intensive care units (ICU) for numbers of purposes. After the placement of a CVL, the confirmation of its proper placement and diagnosis of complications like pneumothoraces are done using chest X-ray (CXR) which is considered the gold standard test. However, this may not always be true. We recently encountered one such case where a dilemma of whether or not to manipulate the central line occurred based on the review of a supine CXR film.A 60-year-old male was posted for craniotomy and excision of a suspected high grade glioma from fronto-parietal region. The case was planned under general anesthesia. A 7F triple lumen CVL was placed under ultrasound guidance in the right internal jugular vein in the supraclavicular approach. As a routine procedure, a call for post-operative CXR was done as the patient was being transferred to the ICU. The CXR was obtained in a semi-sitting position (55 degrees head up) as we suspected a pneumothorax because of the finding of subcutaneous emphysema noted in general examination. Patient remained asymptomatic throughout the night and no chest tube was inserted. A CXR in supine position was obtained the next day. We noted a significant difference in the location of the tip of the CVL as we could see the tip of the catheter at level of 5th rib in semi-sitting position whereas the tip was seen between 6th and 7th rib in the supine position. This led to a confusion to whether we should withdraw the catheter or not. However, we decided to consider the CXR obtained in semi-sitting position to be accurate one and didn’t manipulate the CVL (Figure 1).
We need alternative methods for confirmation
Since the placement of central lines is invasive procedure and these lines lie in close proximity to vital structures, complications or misplacements often result into life-threatening misfortunes. The use of ultrasound as opposed to the historical landmark technique has significantly reduced the rates of these inadvertent misadventures (1). Table 1 highlights results of some of the studies where contrast methods for confirmation of CVL tip were used.

Full table
However, we are far from obtaining an ideal technique to exclude these altogether. It is, therefore, imperative to have a confirmation of proper placement of central lines, or misplacements thereof. Point of care CXR is currently considered the gold standard method for such intent (5). The easy availability and relatively prompt acquisition of image in the patient’s bedside are some of few advantages of a portable CXR. Although portable CXRs are free from alteration of findings due to operator (mis)interpretation like an ultrasound, the technical and non-technical complexities that come with portable CXR images are sometimes bewildering (6). It is, thus, very important to accurately interpret the findings of a supine CXR film.
In an ICU, OT (or other departments with critical care and bed ridden patients), it is often difficult to position the patient in sitting or semi-sitting position for an ideal X-ray film. Therefore, we have to depend upon a supine portable film of chest in order to diagnose a chest pathology or for CVL confirmation. By one definition which states ‘gold standard’ as the most accurate test possible without restrictions, a computed tomography (CT) scan may be considered so for CVL confirmation. However, the cost, relative inaccessibility in ICU or OT, and the need for patient transfer to CT rooms often make CT scan after CVL an unfavorable choice.
Although a supine AP view of CXR may be inferior to an ideal yet difficult-to-obtain PA erect or sitting view, it is still considered accurate enough to diagnose the CVL tip position and is often considered a benchmark test against which other methods of accuracy estimation are compared (7). For emergency department, or ICU physicians and anesthesiologists, these views have always been the only reliable way of confirmation of CVL. The consequences of a CVL placed too deep inside the right atrium or sometimes into right ventricle are grave and include fatal arrhythmias (8).
However, a reliance on a portable supine antero-posterior (AP) CXR is often compounded by several problems like obtaining a reliably accurate position each time the CXR is done, obstruction by several lines like drains, ECG electrodes and wires, nasogastric and orogastric tubes, complicated by inability to inspire and maintain inspiration in case of critical patients, abdominal cavity pushing up on diaphragm restricting the full inspiration, and difficulties in interpretation of the results. Given the fact that an erect/sitting AP or PA view of CXR is more accurate than a supine AP view, the reliance on a portable supine film for confirmation is definitely associated with some discordance.
But this experience of us incites a thought upon whether or not to continue with our reliance on a supine CXR film for confirmation of CVL as it is bound to be associated with technical fallacy resulting into misinterpretation of results which can have serious upshot. This also provokes all of us to explore new alternatives to this reliance. In our case, this deviation was later sorted out with a noble yet experimental method of using agitated saline as contrast agent under ultrasound guidance for confirmation of accurate placement and it revealed that the tip was appropriately located.
Ours’ is not a standalone case depicting the possible problem with a post-CVL placement CXR (9) and we cannot disregard the fact of misrepresentation of correctly located catheter tip by the supine CXR as the gravity of such consequences are unforgiving. However, we would like to recommend either all the X-rays be obtained in sitting/semi-sitting/erect position which at present seems a far-fetched idea especially in setups like ICU or to have all the CXR be reported by a radiologist which, although feasible, is still time-consuming and will delay the management of patient’s conditions or we will have to double-check every CVL thus placed for their accurate location by use of other noble ideas like the agitated saline confirmation for now. We hope that this example of ours, although just one, may encourage all of us to rethink before making an interpretation about the CVL tip simply by looking at a portable supine CXR film. Anonymity and confidentiality regarding patient identification and treatment has been maintained during the writing of this manuscript.
Acknowledgements
Great thanks to Dr. Kishor Khanal, MD for his constant inspiration to this writing.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sazdov D, Srceva MJ, Todorova ZN. Comparative Analysis of Ultrasound Guided Central Venous Catheterization Compared to Blind Catheterization. Pril 2017;38:107-14. (Makedon Akad Nauk Umet Odd Med Nauki). [PubMed]
- Vezzani A, Brusasco C, Palermo S, et al. Ultrasound localization of central vein catheter and detection of postprocedural pneumothorax: an alternative to chest radiography. Crit Care Med 2010;38:533-8. [Crossref] [PubMed]
- Cortellaro F, Mellace L, Paglia S, et al. American Journal of Emergency Medicine Contrast enhanced ultrasound vs chest X-ray to determine correct central venous catheter position. Am J Emerg Med 2014;32:78-81. [Crossref] [PubMed]
- Weekes AJ, Johnson DA, Keller SM, et al. Central Vascular Catheter Placement Evaluation Using Saline Flush and Bedside Echocardiography. Acad Emerg Med 2014;21:65-72. [Crossref] [PubMed]
- Bodenham A, Babu S, Bennett J, et al. GUIDELINES AAGBI: safe vascular access 2016. London: The Association of Anaesthetists of Great Britain & Ireland, 2016.
- Jensen L, Meyer C. Reducing errors in portable chest radiography. Appl Radiol 2015;44:7-15.
- Duran-gehring PE, Guirgis FW, Mckee KC, et al. American Journal of Emergency Medicine The bubble study : ultrasound con fi rmation of central venous. Am J Emerg Med 2015;33:315-9. [Crossref] [PubMed]
- Gapp J, Krishnan M, Ratnaraj F, et al. Cardiac Arrhythmias Resulting from a Peripherally Inserted Central Catheter: Two Cases and a Review of the Literature. Cureus 2017;9:e1308. [PubMed]
- Ergul AB, Ozcan A, Torun YA. Hydrothorax caused by catheter malposition misdiagnosed via using plain radiography. J Turgut Ozal Med Cent 2017;24:354-6.
Cite this article as: Sharma A, Sharma A, Aryal D. Is chest X-ray in supine position for central lines confirmation a gold standard or a fallacy? J Emerg Crit Care Med 2018;2:33.