
Relapsing polychondritis restricted to respiratory tract
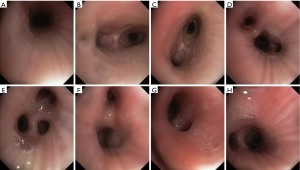
A 38-year-old male was admitted to our emergency department duo to recurrent attacks of breathlessness and chest congestion for 1 year. His medical history included ocular inflammation and arthritis for 5 years. On physical examination, a hoarse voice was clearly heard and respiratory rate was 40 per minute. Tracheal stenosis with thickening wall of it could be found in chest CT scan (Figure 1A,B,C,D,E). Tracheal cartilage revealed disappeared through bronchoscopy (Figures 1F,G,S1). Relapsing polychondritis (RP) was diagnosed and 500 mg of methylprednisolone for 3 days followed by 40 mg of oral prednisone per day was prescripted. The patient has been in good health without a recurrence for 6 months.
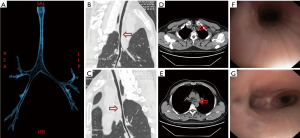
RP is a rare autoimmune disease and only 10% of it can invade the respiratory tract. Any three of the following features including nonerosive seronegative inflammatory arthritis, ocular inflammation, nasal chondritis, bilateral auricular chondritis, audiovestibular damage or respiratory tract chondritis can establish the diagnosis. The prime treatment of RP is glucocorticoid therapy. Methylprednisolone initially loading dose (15 mg/kg/day) is often needed and oral glucocorticoid therapy (1 mg/kg/day) should be lasted for 3–4 weeks. Intubation or tracheotomy might be an alternative in case of emergency. If glucocorticoid therapy doesn’t work well, stent is another option.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Consent was obtained for the use of information and images. The patient’s identity has been kept confidential.
Cite this article as: Zhu C, Yu Y. Relapsing polychondritis restricted to respiratory tract. J Emerg Crit Care Med 2018;2:64.


