An advanced practice registered nurse (APRN)-led initiative to improve post-splenectomy education and vaccine follow-up in adult trauma patients
The spleen the one of the most commonly injured abdominal organs. Damage occurs by direct mechanical impact or shearing from rapid deceleration of the moveable, solid organ against its fixed attaching ligaments causing bleeding into the abdomen (1). A hemodynamically unstable trauma patient demonstrating signs of hemorrhagic shock from abdominal bleeding will undergo exploratory laparotomy early in resuscitation to identify and halt the source of bleeding. When the spleen is the source, prompt surgical removal can be life-saving. Approximately 20–40% of patients with splenic injury require surgery. In up to 60% of blunt abdominal trauma, the spleen is the only organ injured (2).
When functioning normally, the spleen supports immunity by removing particulates such as opsonized bacteria or antibody-coated cells as well as senescent and damaged red blood cells from the blood stream. It clears encapsulated bacteria, which are primarily responsible for a rare but rapidly progressing and highly lethal septicemia in asplenic patients. Despite this well-known mortality risk, many post-splenectomy patients are unaware of their risk and fail to get preventative vaccines (3). Trauma patients are a population generally known for poor rates of follow-up (4). This combination of factors creates a challenge for trauma providers that can potentially be impacted during hospitalization.
Overwhelming post-splenectomy infection (OPSI)
OPSI refers to overwhelming post-splenectomy infection with fulminating sepsis, meningitis, or pneumonia triggered most commonly by three polysaccharide encapsulated bacteria: Streptococcus pneumoniae, Haemophilus influenzae type B and Neisseria meningitidis. The prevalence of OPSI after splenectomy from trauma is reported at 2.3%, however it is likely higher when tracked over the lifetime (5). Risk of OPSI in asplenic patients is fifty times greater than the general population with S. pneumoniae the causal organism in 50–90% of cases followed by H. influenzae B, then N. meningitides (5,6). OPSI is a medical emergency presenting with vague symptoms of fever, rigors, myalgia, headache, vomiting and diarrhea. Septic shock develops within hours and is quickly followed by anuria, hypotension, hypoglycemia, disseminated intravascular coagulopathy, then multi-organ failure and death (3). Treatment includes early antibiotics, typically third generation cephalosporins, and supportive care. The mortality in OPSI is an alarming 50–80% and most deaths occur in the first 24 hours of symptom onset, even when identified and treated aggressively in a modern ICU (6,7).
Vaccination
Immunization against the common organisms is the primary protective mechanism against infectious complications in adults who have undergone splenectomy. While it does not eliminate the risk, it reduces the occurrence of OPSI in asplenic patients (8). The United States Advisory Committee on Immunization Practices (ACIP) recommends vaccination against the most common pathogens responsible for OPSI (9-12) (Table 1). In 2012, changes were made to the ACIP pneumococcal recommendations to include the pneumococcal 13-valent conjugate vaccine (PCV 13) initially for asplenic adults, followed by the pneumococcal 23-valent polysaccharide vaccine (PPSV 23) after 8 weeks (10). Although the PCV 13 includes fewer serotypes, it has superior immunogenicity and the combination confers optimal protection. The recent addition of the meningococcal serogroup B series in 2015 now requires the patient to return twice for vaccines after discharge (12). Many studies find that patients are often undereducated about their risk of OPSI and do not receive the recommended vaccines even in ideal circumstances with high quality universal healthcare and centralized vaccine registries (7,13-15). The difference in risk associated with poor compliance with a vaccine series versus one-time dosing is not discussed in the recommendations.

Full table
Education and self-care
OPSI is a rare but serious lifetime risk which patients must remain vigilant for concerning symptoms. Targeted patient education delivered during teachable moments after trauma can significantly improve patient’s health behaviors post-discharge (8,16). A large study, however, found that 84% of patients who have undergone splenectomy were unaware of their increased susceptibility to severe infection or of the need for vaccines (3). Additional studies specifically addressing traumatic splenectomy populations show similar discouraging trends of adherence to post-splenectomy instructions (17,18). Authors suggest that better education and tracking of these patients may improve compliance. Promoting a patient’s ability and motivation to develop positive health behaviors aligns with a leading theory of nursing practice. Orem’s theory of self-care assumes all people innately desire self-care agency, and that self-care is a learned behavior (19). When disease or injury creates a deficit in a person’s independence, they overcome or adapt through direct care and education provided by the health system. Orem’s theory further holds that the role of nursing is to facilitate return to self-care for the patient, and to provide knowledge and support to protect themselves from infection (19).
This trauma center underwent a quality improvement project to standardize post-splenectomy care by ensuring all patients received correct vaccines in the hospital; consistently delivering education highlighting severity of risk and symptoms of infection; and, making a precise plan for vaccine follow-up with printed take-home materials and vaccine reminders. The primary aim was to ensure vaccine delivery and discharge education in newly asplenic patients at our trauma center. The secondary aim was to prevent OPSI in the same population.
Methods
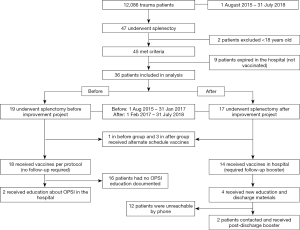
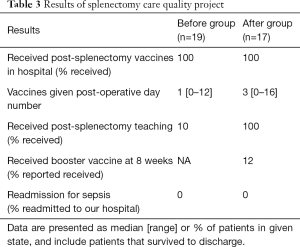
The setting is a 540-bed county-owned academic level 1 trauma center in a metropolitan city of approximately 2 million residents. There is a robust multi-specialty resident workforce on the trauma ICU and trauma surgery floor services. Prior to the change, post-splenectomy patients were given a one-time set of 3 vaccines (PPSV 23, meningococcal conjugate, and Hib) during their hospitalization. This schedule did not require follow-up vaccines and infection prevention teaching was done by the primary nurse or junior resident discharging the patient. There was no standard plan for delivery or documentation of patient education, no materials for the patient to take home and no advanced practice registered nurses (APRN) on either service at this time. Two APRNs were added to the service just prior to this project, they assumed responsibility for discharge instruction and took the lead implementing this change. The quality improvement project followed a simple four step model (Figure 1). First standardize vaccine practice to evidence-based guidelines, design a simple teaching plan, provide patients with a precise plan for follow-up, and confirm adherence with post-discharge phone communication. Eighteen months of data was collected post-implementation and compared with the previous 18 months data prior to the change. Before and after data were analyzed using descriptive statistics.
Standardize vaccine practice
A multidisciplinary group convened to implement this change including trauma APRNs, trauma surgeon champion, infectious disease physician, clinical pharmacist, and trauma nursing leadership. This core group planned the timeline and preparatory milestones necessary to begin the project. These were to build orders in the electronic medical record (EMR), ensure purchase and adequate stock the correct vaccines in the units, create teaching plan and materials, and present the project to stakeholders to obtain buy-in. Each workgroup member made their department aware of the change and brought forward concerns. As there were multiple disciplines involved, much constructive discussion ensued during the buy-in phase regarding the best approach to achieve optimal adherence and outcomes. When the plan was finalized, resident physicians, trauma nurses and clinical pharmacists received education on the new protocol and patient teaching plan.
Create simple and consistent patient education
Patient education focused on three messages: severity of OPSI; importance of vaccines; and signs of infection requiring immediately medical care. Resident physicians, advanced practitioners and critical care nurses were comfortable with this message and were empowered to deliver it in a teaching style that was best individualized to the patient. For patients who were not alert and oriented, teaching was provided to their primary caregiver.
Provide patients with a precise plan for follow-up
A reminder handout was created and given to the patient during the education. It is simply written and provides date of operation, date of initial vaccination, and due dates for follow-up vaccines. A plan was made to see their primary care provider or obtain vaccines from a local health department. Cost of the vaccine for patients without insurance was discussed to prepare them, and help to obtain discounts.
Confirm adherence with phone communication
Follow-up phone calls, when possible, were attempted to confirm vaccine follow-up and reinforce education post-discharge.
Results
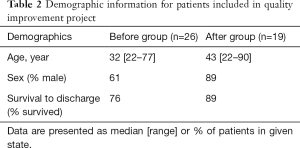
A total of 12,086 trauma patients were observed from August 2015–July 2018. Three years of data was collected in equal time periods before and after the intervention. The after group had fewer female patients and better survival to discharge (Table 2). A total of 36 adult patients underwent splenectomy and were included in the analysis (Figure 2) (Table 3). All patients who survived to discharge received vaccines in the hospital. The vaccine schedule given to patients in the before group was a one-time dose and did not require booster. Review of discharge documentation showed only 10% had education documented about risk of OPSI and symptoms of infection before the intervention and 100% received education in the after group. Fourteen patients in the after group received the new schedule vaccines requiring booster at 8 weeks. Two (12%) patients reported they received vaccines, though 12 were unable to be contacted. The resident and APRN staff consistently adhered to the change in practice. There were no re-admissions for OPSI for either group during the study period.
Full table
Full table
Discussion
APRN role
In the role of lead change agent, the APRN is uniquely positioned to collaborate with the multidisciplinary stakeholders, and oversee the daily operation of the practice change involved in this quality project. As a consistent provider presence on the trauma service trained in the nursing theoretical basis, the APRNs taught the resident physicians and nurses in real-time and ensured continuity for the duration of the project.
Decreases in splenectomy
In our sample, a 25% decrease in splenectomy occurred between the before and after group despite a 14% increase in overall trauma volume with 5,659 trauma patients in before group and 6,427 in after group. This trend is possibly related to change in practice over time and limits the before/after comparison. The use of non-operative management and spleen-sparing procedures such as spleen embolization is increasing and consequently, the number of splenectomies is decreasing. It is reported that nearly 50–70% of splenic injury are now managed with observation or embolization techniques (20). There is evidence that residual functional splenic tissue in the body may abrogate the risk of OPSI and by extension the need for vaccination (21). It is unclear whether vaccination benefits these patients and little consensus exists among trauma surgeons (22,23). Current practice at our center is generally to vaccinate patients who have a proximal embolization of the splenic artery or are otherwise rendered more than 50% functionally asplenic. We look for more data on OPSI in these populations to guide future practice.
Challenges of trauma follow-up
Results confirm those in the literature regarding difficulty contacting and following-up in the trauma population post-discharge. Of the 14 patients requiring follow-up, 12 were unable to be contacted for various reasons such as a change in phone number or no number available. Occasionally the severity of the trauma caused a profound change in the patient’s independence related to cognitive/functional status, preventing a return to previous levels of self-care. It is unclear whether the unreachable patients received follow-up vaccines. Many authors suggest a centralized electronic registry as a way to track patients and remind them to obtain follow-up vaccines, though there are few feasible ways to accomplish this in our current electronic infrastructure. The Veterans Administration (VA) is one such large health system in the US that has an electronic system capable of tracking long-term adherence to follow-up. The VA achieved significant increases in post-splenectomy vaccine compliance using a travel clinic staffed by nurse practitioners tracking splenectomy patients lost to follow-up (24). With the right resources these results could potentially be translated to the general population as well. It was noted that 6 of the 12 patients who were unable to be contacted by phone visited the hospital for other reasons after 8 weeks, and in 3 cases were admitted to another service. No notification currently exists in the EMR when a vaccine is due, but a simple electronic trigger would have easily allowed administration of follow-up vaccines during a subsequent visit.
Strong teams of trauma clinicians ensure that vaccines and educational interventions are delivered in hospital even as rates of splenectomy decline. The impact of the critical care nurse in these discussions cannot be overstated with patients and families. In parallel with teaching by the physician or APRN, the nurse often has opportunity to reinforce education and offer advice at precise teachable moments. It is known that simply improving patient education alone does not consistently improve compliance and there are complex socioeconomic factors that influence patients’ health behaviors (25). Based on self-care theory, when a patient is given the correct knowledge and support, they are able to manage their life, health and wellbeing on their own behalf (26). For this reason, a theory-based approach was chosen to discuss OPSI in the ICU, deliver practical information about dates and locations, and be fully transparent about cost to facilitate optimal self-care.
In conclusion, we found that a quality improvement project could achieve high rates of post-splenectomy vaccination in hospital, but opportunity exists to find ways to ensure patients are compliant with booster vaccines after discharge from the hospital. While no patients were readmitted for sepsis during this study period at our hospital, OPSI is a lifelong risk and most patients’ current health status is unknown. The small scope of this project limited our ability draw reliable conclusions, but continued tracking of these patients may tell us which, if any, of these interventions make an impact on health-related behaviors.
Acknowledgements
The author would like to acknowledge asplenia workgroup: S Asad, MD; A Chavarria, APRN; F Simon, PharmD; and the trauma surgeons with the UNLV School of Medicine for their support of this quality improvement project.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Informed Consent: The protocol for this project was approved by the IRB for University Medical Center of Southern Nevada and met requirements for waiver of informed consent.
References
- ATLS Subcommittee; American College of Surgeons’ Committee on Trauma; International ATLS working group. Advanced Trauma Life Support (ATLS®): the ninth edition. J Trauma Acute Care Surg 2013;74:1363-6.
- Davis JJ, Cohn I Jr, Nance FC. Diagnosis and management of blunt abdominal trauma. Ann Surg 1976;183:672. [Crossref] [PubMed]
- Brigden ML, Pattullo AL. Prevention and management of overwhelming postsplenectomy infection-an update. Crit Care Med 1999;27:836-42. [Crossref] [PubMed]
- Stone ME Jr, Marsh J, Cucuzzo J, et al. Factors associated with trauma clinic follow-up compliance after discharge: experience at an urban Level I trauma center. J Trauma Acute Care Surg 2014;76:185-90. [Crossref] [PubMed]
- Hansen K, Singer DB. Asplenic-hyposplenic overwhelming sepsis: postsplenectomy sepsis revisited. Pediatr Dev Pathol 2001;4:105-21. [Crossref] [PubMed]
- Holdsworth RJ, Irving AD, Cuschieri A. Postsplenectomy sepsis and its mortality rate: actual versus perceived risks. Br J Surg 1991;78:1031-8. [Crossref] [PubMed]
- Boam T, Sellars P, Isherwood J, et al. Adherence to vaccination guidelines post splenectomy: A five year follow up study. J Infect Public Health 2017;10:803-8. [Crossref] [PubMed]
- El-Alfy MS, El-Sayed MH. Overwhelming postsplenectomy infection: is quality of patient knowledge enough for prevention? Hematol J 2004;5:77-80. [Crossref] [PubMed]
- Briere EC, Rubin L, Moro PL, et al. Prevention and control of haemophilus influenzae type b disease: recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep 2014;63:1-14. [PubMed]
- Centers for Disease Control and Prevention (CDC). Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 2012;61:816-9. [PubMed]
- Cohn AC, MacNeil JR, Clark TA, et al. Prevention and control of meningococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2013;62:1-28. [PubMed]
- Folaranmi T, Rubin L, Martin SW, et al. Use of Serogroup B Meningococcal Vaccines in Persons Aged ≥10 Years at Increased Risk for Serogroup B Meningococcal Disease: Recommendations of the Advisory Committee on Immunization Practices, 2015. MMWR Morb Mortal Wkly Rep 2015;64:608-12. [PubMed]
- Luu S, Dendle C, Jones P, et al. Impact of a spleen registry on optimal post-splenectomy vaccination and care. Hum Vaccin Immunother 2018;18:1-6. [Crossref] [PubMed]
- Di Sabatino A, Lenti MV, Tinozzi FP, et al. Vaccination coverage and mortality after splenectomy: results from an Italian single-centre study. Intern Emerg Med 2017;12:1139-47. [Crossref] [PubMed]
- Kotsanas D, Al-Souffi MH, Waxman BP, et al. Adherence to guidelines for prevention of postsplenectomy sepsis. Age and sex are risk factors: a five-year retrospective review. ANZ J Surg 2006;76:542-7. [Crossref] [PubMed]
- Field C, Walters S, Mari N, et al. A multisite randomized controlled trial of brief intervention to reduce drinking in the trauma care setting. Ann Surg 2014;259:873-80. [Crossref] [PubMed]
- Carrico RM, Goss L, Wojcik J, et al. Postsplenectomy vaccination guideline adherence: opportunities for improviement. J Am Assoc Nurse Pract 2017;29:612-7. [Crossref] [PubMed]
- Alvarado AR, Udobi K, Berry S, et al. An opportunity for improvement in trauma care: 8-week booster vaccination adherence among patients after trauma splenectomy. Surgery 2018;163:415-8. [Crossref] [PubMed]
- Orem DE. Nursing: Concepts of Practice. McGraw Hill, New York, 2001.
- McIntyre LK, Schiff M, Jurkovich GJ. Failure of nonoperative management of splenic injuries: causes and consequences. Arch Surg 2005;140:563-8; discussion 568-9. [Crossref] [PubMed]
- Demetriades D, Scalea TM, Degiannis E, et al. Blunt splenic trauma: splenectomy increases early infectious complications: a prospective multicenter study. J Trauma Acute Care Surg 2012;72:229-34. [Crossref] [PubMed]
- Shatz DV. Vaccination practices among North American trauma surgeons in splenectomy for trauma. J Trauma 2002;53:950-6. [Crossref] [PubMed]
- Di Sabatino A, Carsetti R, Corazza GR. Post-splenectomy and hyposplenic states. Lancet 2011;378:86-97. [Crossref] [PubMed]
- Mitchell AP, Boggan JC, Lau K, et al. Splenectomy as a Destination: Improving Quality of Care Among Asplenic Veterans Through a Travel Clinic. Am J Med 2017;130:856-61. [Crossref] [PubMed]
- Nweze IC, DiGiacomo JC, Shin SS, et al. Demographic and socioeconomic factors influencing disparities in prevalence of alcohol-related injury among underserved trauma patients in a safety-net hospital. Injury 2016;47:2635-41. [Crossref] [PubMed]
- Khatiban M, Shirani F, Oshvandi K, et al. Orem's Self-Care Model With Trauma Patients: A Quasi-Experimental Study. Nurs Sci Q 2018;31:272-8. [Crossref] [PubMed]
Cite this article as: Andersen A. An advanced practice registered nurse (APRN)-led initiative to improve post-splenectomy education and vaccine follow-up in adult trauma patients. J Emerg Crit Care Med 2018;2:104.