
Terlipressin for septic shock patients: protocol for a systematic review and meta-analysis
Introduction
Septic shock is life-threatening and refractory vasodilatory shock in intensive care unit (ICU). Vasopressor therapy is crucial in the management of septic shock to achieve target arterial blood pressure. Catecholamine has long been first and foremost recommended vasopressors (1). However, some patients may remain refractory to this agent, which is also known as catecholamine-resistant septic shock (2,3). Moreover, high-dose catecholamine therapy may lead to potential side effects such as increased myocardial oxygen consumption, lethal arrhythmias and even high risk of mortality (4). Thus, selection of other vasoactive drugs as alternative or accessory that may benefit septic shock while avoiding unnecessary side effects is important.
Vasopressin is an endogenously released peptide hormone and exerts vasoconstriction effect via stimulating specific receptors mainly V1 receptors (5-7). Previous studies indicated survival benefit in terlipressin (8). Recent guideline also referred the use of vasopressin as potential rescue agents in catecholamine-refractory septic shock (1). However, in a previous randomized controlled trial (RCT), low-dose arginine vasopressin (AVP) showed no survival benefit in comparison with norepinephrine for septic shock patients (6). One of potential explanation for this is that vasopressin has no selectivity for V1 receptors and may also active other receptors, thus leading to a variety of adverse effects, such as decreased cardiac output, thrombocytopenia, hyponatremia or hyperbilirubinemia (5-7). Therefore, terlipressin (tricyl-lysine vasopressin), a synthetic analog of vasopressin, has attracted attention for its similar pharmacodynamic profile but greater selectivity of V1 receptor (5-7).
Terlipressin was evaluated in the subgroup of the previous meta-analyses of vasopressin/terlipressin therapy for vasodilatory shock (8-10), and showed no survival benefit. However, two of the previous meta-analyses (8,9) included only three RCTs evaluating terlipressin (11-13), and some of important outcomes such as effect on the dose of catecholamine, duration of mechanical ventilation (MV) and length of stay (LOS) in ICU or hospital were not considered (12,13); only neonatal and pediatric population subjected to the third meta-analysis (10). Another meta-analysis compared various kinds of vasopressors with arms of norepinephrine, epinephrine, vasopressin/terlipressin, dopamine, phenylephrine and placebo, implied no difference in mortality between norepinephrine and vasopressin/terlipressin however, terlipressin was neither analyzed at full length nor pooled separately from vasopressin (14). Several RCTs have been published after the year of 2010 (2,8,15-19), including the ever-largest trial on terlipressin published in 2018 (19), however, the updated data have not been meta-analyzed yet. Thus, we aim to conduct a meta-analysis to further investigate the efficacy and safety of terlipressin for septic shock.
Review question
Is terlipressin an effective substitute for catecholamines in septic shock patients?
Methods and analysis
Registration
The study was registered on the PROSPERO registration website (CRD42018104924). The review protocol was conducted according to the PRISMA-P guidance (20).
Search methods
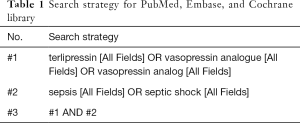
Three separate electronic data sources (Embase, PubMed and Cochrane database) from inception through July 15, 2018 to identify potentially relevant RCTs with no language restriction. In addition, reference lists will be searched manually. A search strategy was developed for the three databases and consisted of terms related to septic shock and terlipressin (Table 1).
Full table
Study inclusion criteria
Studies to be included
We will include studies meeting the following criteria: (I) RCTs; (II) ICU patients with septic shock; (III) intervention: patients receiving terlipressin, regardless of dosage, frequency, duration and administration routes; any open-label catecholamines can be added whenever needed; (IV) control: patients receiving any catecholamines; (V) reporting any of the following outcomes: mortality, ICU-LOS, duration of MV, catecholamines requirement, lactate clearance, and adverse events (AEs). Studies will be excluded if they enrolled pregnant or breastfeeding woman, or if they were only in abstract form, meeting reports.
Intervention
Terlipressin for vasopressive therapy; the administration routes including intermittent bolus and/or continuous intravenous infusion; the administration strategies including giving a fixed dose and/or titrating to achieve target arterial blood pressure.
Comparison
Catecholamines including norepinephrine, epinephrine, dopamine, dobutamine used for vasopressive therapy.
Outcome
The primary outcome is all causes mortality at the longest follow up available. Secondary outcomes include ICU-LOS, duration of MV, catecholamines requirement, and AEs.
Data collection and analysis
Selection of studies
The two reviewers (H Huang, Y Zhu) will screen the search results independently according to the title and abstract. After the full paper obtained, the two reviewers will screen the references for potentially relevant studies. Any disagreements will be solved by discussion with a third author (Y Wang). We will contact the authors if any further information is needed. The study selection process will be summarized and reported as a flow chart.
Data extraction and management
The two reviewers (H Huang, Y Zhu) will independently extract data from each included RCT and fulfill a data extraction form with the information of the study name, publication date, study design, setting, sample size, treatment algorithms of terlipressin and control groups, prognostic index, methodological quality, and relevant outcomes.
Assessment of the quality of included studies
We will use the Cochrane Collaboration’s tool to assess risks of selection bias, performance bias, attrition bias, reporting bias and other bias for each included RCT (21). A statistical expert (Y Wang) will be consulted to solve any discrepancies.
Statistical analysis and data synthesis
All analyses will be performed using Review Manager, Version 5.3. The pooled effects will be analyzed using risk ratio (RR) for dichotomous outcomes, and weighted mean differences (WMDs) for continuous outcomes, with 95% confidence intervals (CIs). If any RCT reported only median and interquartile range (IQR) rather than mean and standard deviation (SD), we will estimate mean and SD using the method described in previous studies (22).
Assessment of heterogeneity
Statistical heterogeneity will be tested by using the I2 statistic. Clinical heterogeneity will be considered and discussed by the two authors (H Huang, Y Zhu) and the two clinical experts (B Du, X Xi). We will use fixed effect model when there is negligible heterogeneity. A random effect model will be used if there is significant clinical and/or statistical heterogeneity.
Subgroup analyses
We will conduct subgroup analyses to test the robustness of our primary outcome and to further explore the potential influence factors. Subgroups will include: (I) type of catecholamine as control (norepinephrine or other catecholamines); (II) administration of terlipressin (bolus or continuous); (III) terlipressin dose (>4 mg/day; 2–4 mg/d or <2 mg/day); (IV) study design (blinded or unblinded); (V) published year (before year 2010 or after year 2010).
Sensitivity analyses
For our primary outcome measure, mortality, sensitivity analyses will be conducted through groups of: (I) 28-day mortality; (II) ICU mortality; (III) hospital mortality; (IV) more severe septic shock (defined as catecholamine-resistant septic shock or patients received more than 15ug/min norepinephrine at randomization); (V) studies of exclusion of the largest trial; (VI) studies of exclusion of pediatrics.
Publication bias
Funnel plots will be used to evaluate publication bias when at least ten RCTs are included.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The present meta-analysis is based on published data and thus no specific ethical clearance is required. The results of this meta-analysis will be published in a peer-reviewed journal.
References
- Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med 2017;43:304-77. [Crossref] [PubMed]
- Svoboda P, Scheer P, Kantorová I, et al. Terlipressin in the treatment of late phase catecholamine-resistant septic shock. Hepatogastroenterology 2012;59:1043-7. [PubMed]
- Leone M, Boyle WA. Decreased vasopressin responsiveness in vasodilatory septic shock-like conditions. Crit Care Med 2006;34:1126-30. [Crossref] [PubMed]
- Schmittinger CA, Torgersen C, Luckner G, et al. Adverse cardiac events during catecholamine vasopressor therapy: a prospective observational study. Intensive Care Med 2012;38:950-8. [Crossref] [PubMed]
- Torgersen C, Dünser MW, Wenzel V, et al. Comparing two different arginine vasopressin doses in advanced vasodilatory shock: a randomized, controlled, open-label trial. Intensive Care Med 2010;36:57-65. [Crossref] [PubMed]
- Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med 2008;358:877-87. [Crossref] [PubMed]
- Salazar M, Hu BB, Vazquez J, et al. Exogenous Vasopressin-Induced Hyponatremia in Patients With Vasodilatory Shock: Two Case Reports and Literature Review. J Intensive Care Med 2015;30:253-8. [Crossref] [PubMed]
- Serpa Neto A, Nassar AP, Cardoso SO, et al. Vasopressin and terlipressin in adult vasodilatory shock: a systematic review and meta-analysis of nine randomized controlled trials. Crit Care 2012;16:R154. [Crossref] [PubMed]
- Polito A, Parisini E, Ricci Z, et al. Vasopressin for treatment of vasodilatory shock: an ESICM systematic review and meta-analysis. Intensive Care Med 2012;38:9-19. [Crossref] [PubMed]
- Masarwa R, Paret G, Perlman A, et al. Role of vasopressin and terlipressin in refractory shock compared to conventional therapy in the neonatal and pediatric population: a systematic review, meta-analysis, and trial sequential analysis. Crit Care 2017;21:1. [Crossref] [PubMed]
- Morelli A, Ertmer C, Lange M, et al. Effects of short-term simultaneous infusion of dobutamine and terlipressin in patients with septic shock: the DOBUPRESS study. Br J Anaesth 2008;100:494-503. [Crossref] [PubMed]
- Albanèse J, Leone M, Delmas A, et al. Terlipressin or norepinephrine in hyperdynamic septic shock: a prospective, randomized study. Crit Care Med 2005;33:1897-902. [Crossref] [PubMed]
- Yildizdas D, Yapicioglu H, Celik U, et al. Terlipressin as a rescue therapy for catecholamine-resistant septic shock in children. Intensive Care Med 2008;34:511-7. [Crossref] [PubMed]
- Avni T, Lador A, Lev S, et al. Vasopressors for the Treatment of Septic Shock: Systematic Review and Meta-Analysis. PLoS One 2015;10:e0129305. [Crossref] [PubMed]
- Hua F, Wang X, Zhu L. Terlipressin decreases vascular endothelial growth factor expression and improves oxygenation in patients with acute respiratory distress syndrome and shock. J Emerg Med 2013;44:434-9. [Crossref] [PubMed]
- Xiao X, Zhang J, Wang Y, et al. Effects of terlipressin on patients with sepsis via improving tissue blood flow. J Surg Res 2016;200:274-82. [Crossref] [PubMed]
- Chen Z, Zhou P, Lu Y, et al. Comparison of effect of norepinephrine and terlipressin on patients with ARDS combined with septic shock: a prospective single-blind randomized controlled trial. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2017;29:111-6. [PubMed]
- Choudhury A, Kedarisetty CK, Vashishtha C, et al. A randomized trial comparing terlipressin and noradrenaline in patients with cirrhosis and septic shock. Liver Int 2017;37:552-61. [Crossref] [PubMed]
- Liu ZM, Chen J, Kou Q, et al. Terlipressin versus norepinephrine as infusion in patients with septic shock: a multicentre, randomised, double-blinded trial. Intensive Care Med 2018;44:1816-25. [Crossref] [PubMed]
- Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [Crossref] [PubMed]
- Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [Crossref] [PubMed]
- Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135. [Crossref] [PubMed]
Cite this article as: Zhu Y, Huang H, Wang Y, Zhang L, Xi X, Du B. Terlipressin for septic shock patients: protocol for a systematic review and meta-analysis. J Emerg Crit Care Med 2018;2:108.


