
Idiopathic intrahepatic arterioportal shunt rupture
A 70-year-old Thai female end-stage renal disease (ESRD) patient, with a 4 years history of peritoneal dialysis, was brought to the emergency department because of syncope after her regular peritoneal dialysis, and a mixture of fluid and blood was obtained from the peritoneal fluid. Blood loss was suspected from her physical examinations and labs. Her past medical history showed hypertension, dyslipidemia, ischemic stroke, causing right hemiparesis 10 years ago and aspirin (ASA) has been prescribed.
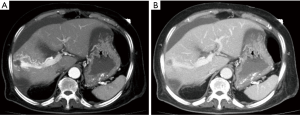
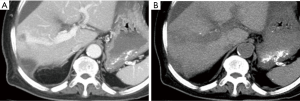
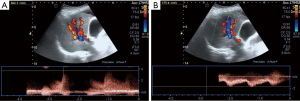
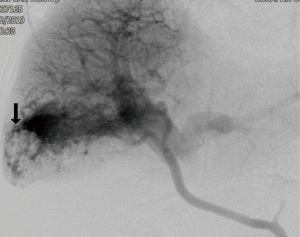
She underwent contrast-enhanced computed tomography (CECT) of the abdomen to evaluate the source of bleeding. Multiphase CECT revealed a large arterioportal shunt (APS) at right hepatic lobe (Figures 1,2). A large hemoperitoneum was noted however, there was no active contrast extravasation. Color Doppler ultrasound (CDU) was subsequently performed. Multiple enlarged feeding right hepatic artery branches were noted with high velocity as well as a large draining right portal vein branch (Figure 3). Coagulopathy was developed after admission and fresh frozen plasma was replaced. The patient underwent angiogram with polyvinyl alcohol particles (PVA) embolization on the following day. A selective angiogram revealed high flow APS at posterior segment of right hepatic lobe via multiple abnormal feeding vessels from branches of the right hepatic artery with early venous drainage via right portal vein branches (Figure 4). Residual APS but with the slow flow was noted after embolization by PVA. Nevertheless, the patient’s coagulopathy was not recovered. The patient’s condition was deteriorated. Her offspring denied aggressive treatment and the patient died eventually.
APS of the liver can occur congenitally, acquired after trauma or hepatic intervention, or spontaneously in association with cirrhosis or liver tumors. The idiopathic or congenital type of APS is rare. CECT combined with CDU is sufficient for the diagnosis and planning of the treatment. Embolization or surgical ligation of the hepatic artery is the treatment aimed to close the shunt. Hepatic resection or transplantation is reserved for failure of shunt closure.
Acknowledgments
The authors are grateful to Faculty of Medicine Burapha University for all supports.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient’s offspring for publication of this manuscript and any accompanying images.
Cite this article as: Limchareon S, Ruangsirinusorn W. Idiopathic intrahepatic arterioportal shunt rupture. J Emerg Crit Care Med 2019;3:42.


