Consideration for thrombolysis for significant pulmonary embolism in haemodynamically stable patients—is it time for a rethink?
Introduction
Pulmonary embolism (PE) is a common diagnosis (1) made in the emergency department with 60–70 cases per 100,000. The clinician needs to have UpToDate knowledge and potential treatment strategies for management of this common condition. Thrombolysis for PE is one of the options that can be considered in the Emergency Department. In the patient without haemodynamic stability the situation becomes trickier with some clinicians considering thrombolysis without significant haemodynamic compromise in a preventive measure whilst other purporting its use in peri-arrest and cardiac arrest use. The discussion then becomes whether early treatment is better suited than rescue systemic thrombolysis. The British Thoracic Society (BTS) has formed a set of recommendations for consideration of thrombolysis.
Certain absolute contraindications (2) for thrombolysis are as follows:
- Recent major surgery (>3/12);
- History of previous intracranial haemorrhage;
- Known intracranial malformation or neoplasm;
- Suspected dissection;
- Recent head trauma;
- Bleeding diathesis.
Relative contraindications:
- >75 years of age;
- Current anticoagulants;
- Pregnancy;
- Cardiopulmonary resuscitation >10 min;
- Recent internal bleed (2–4 weeks);
- Uncontrolled hypertension (180/110 mmHg);
- Remote ischaemic stroke;
- Major surgery within 3 weeks.
Case presentation and discussion of findings
We will discuss two clinical cases of differing severity and discuss the rationale behind the treatment strategies.
Firstly, we present a lady in her late 40s with acute shortness of breath with pleuritic chest pain. She was brought in by ambulance and the resuscitation suite was pre-alerted that she was due to arrive. She had been recently treated for a lower limb deep venous thrombosis (DVT) and had presented to a local hospital 2/7 previously with some associated pleuritic chest pain, However, due to logistical restraints her computed tomogram pulmonary angiogram (CTPA) could not be performed on last presentation to her hospital, she had been on dose dalteparin (low molecular weight heparin) since her DVT diagnosis.
On presentation to our Emergency Department she was noted to be profoundly hypoxic with oxygen saturation of 90% on 15 litres of oxygen via a non-breathable mask and was also noted to be compromised from a haemodynamic view (hear rate 120 bpm and systolic blood pressure of 90 mmHg). The hospital pre-alert provided us with valuable information including earlier consideration of the use systemic thrombolysis and the necessary preparation. There was significant cardiovascular and respiratory instability noted on this occasion. The risks of significant haemorrhage were discussed with the patient with verbal informed consent to proceed for systemic thrombolysis.
Some authors may suggest that further investigations including a CTPA would enable the diagnosis to be made. However, it’s worth noting that the lady was in a peri-arrest scenario where time was a critical factor and there was already concerns that she had developed an embolism from the recent DVT. Alteplase is the drug of choice across Emergency Departments across the United Kingdom for systemic thrombolysis for both acute myocardial infarctions not suitable/stable for primary percutaneous coronary intervention and PE. Following systemic thrombolysis with supplemental oxygen therapy given, she made a complete recovery and subsequently discharged home in the next 24 h.
The second case we present is that of a 50-year-old previously fit and well gentleman who presented with acute shortness of breath on minimal exertion for the previous 3 days. There was no background history of airway diseases with no smoking. He was noted to be marked hypoxic requiring 5 litres of oxygen to maintain an oxygen saturation of 95%. On his arterial blood gas his PaO2 was noted to be 8.82 on 5litres of oxygen. He was noted to be persistently tachycardic with a heart rate between 120–125 beats/min with Systolic BP being maintained between 120–130 mmHg throughout his stay in ED. His baseline electrocardiogram was that of sinus tachycardia which later on developed into the rare S1Q3T3 pattern (deep S waves in Lead I, Q waves in Lead III and T wave inversion in lead III). Blood tests indicated a markedly raised D-dimer and also evidence of a markedly raised troponin.
Studies have shown that a raised cardiac troponin (3) (both I and T) in the context of acute PE is associated with RV myocardial injury and predicts both short term mortality and associated complications. This applies in the haemodynamically stable patient as well with high levels of mortality.
However, unlike our previous patient, he was stable to undergo a CTPA. The CTPA revealed large bilateral PE just distal to the bifurcation of the pulmonary artery with evidence of right heart strain.
In the department a bedside echocardiogram also revealed right ventricular strain with a grossly dilated right ventricular without any collapsibility. Whilst supportive treatment was instituted, a discussion was made with the regional cardiothoracic surgeons for consideration for possible surgical embolectomy. Surgical embolectomy is an option especially if patients are carefully selected and especially in patients where thrombolysis is contraindicated. This is often seen as last resort especially if all other options have been tried/not possible including catheter based mechanical clot disruption. The rates of mortality are varied between 6–46% (4,5), in a recent study (6) performed on both haemodynamically stable and unstable patients; the overall operative mortality was noted to be 6.6% (10.2% for unstable patients and 3.6% for stable patients). Following a joint discussion with the cardiothoracic surgeons and the cardiologists, the decision was made for systemic thrombolysis. This treatment decision was then discussed with the patient and his family with discussion of increased bleeding risks and following informed consent systemic thrombolysis was commenced. He was subsequently transferred to our local cardiology unit or ongoing management, unfortunately due to the extent of the PE and the associated complication he developed pulmonary hypertension. He is currently being managed by the cardiologist.
Both our patients would classify as having a massive PE (significant), out first patient was peri-arrest in the department and systemic thrombolysis as indicated. Our second patient had features of massive PE (evidence of right heart strain, raised troponin from RV myocardial damage) even though his blood pressure remained stable throughout.
Discussion
The case for and against systemic thrombolysis
The evidence for systemic thrombolysis in patients with PE without any evidence of haemodynamic compromise is conflicting. In a study undertaken by Konstantinides et al. (7) reports that in patients with acute PE without hypotension but with evidence of RV dysfunction, alteplase reduced the risk of in-hospital death without increasing the chances of major haemorrhagic complications. In studies undertaken by Marti et al. (8) and a meta-analysis done by Chatterjee et al. (9), showed significant reduction in mortality in patients with intermediate-risk PE. It was also noted that that there was no significant difference in outcomes with the type of thrombolytic agents i.e. alteplase, tenecteplase or older thrombolytics.
As a counter argument, some studies have shown that systemic thrombolytics are associated with increased risk of significant haemorrhage. In the PE Thrombolysis (PEiTHO) trial (10) investigators discovered that a single dose of tenecteplase when used in haemodynamically stable patients with acute PE was associated with a high risk of haemorrhagic stroke. In the same study by Marti et al. (8) the risk of significant haemorrhage including intracranial haemorrhage was increased with systemic thrombolysis.
BTS Guidelines (11)
The presence of raised troponin in the presence of an acute PE classifies as a massive PE. Systemic thrombolysis is the first line treatment for massive PE and should be started on clinical grounds alone if cardiac arrest in imminent with alteplase being the drug of choice. Invasive approached including thrombus fragmentation and IVC filter insertion should be considered if the facilities and expertise are available to do so. In our second case, this could have been considered however the expertise was not available to perform this procedure. The gold standard imaging for PE is with a CTPA and a negative CTPA reliably excludes PE. If there is a high clinical probability of a PE, performing a D-dimer is not clinically indicated.
Highlighted points
- CTPA and Echocardiogram are both useful for diagnosis of clinically massive PE;
- Haemodynamic stability is not solely based on blood pressure measurements alone;
- Careful patient selection is required with the appropriate risk stratification;
- Risks of major haemorrhage is increased in patients undergoing systemic thrombolysis;
- Early assessment of right ventricular dysfunction helps to guide prognosis;
- Widespread use with appropriate training of bedside echocardiogram by ED clinicians. The ability to perform echocardiogram in life support is one of the essential skills required of ED clinicians as advised by the Royal College of Emergency Medicine.
Conclusions
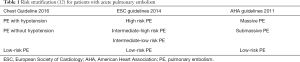
The decision to perform systemic thrombolysis in the haemodynamically stable patient is multifactorial and should be assessed in a case by case manner as highlighted by this article. Patients should be consented about the risks of haemorrhage associated with systemic thrombolysis. Early diagnosis and management are key to ensure optimise survival risk. For massive PE, systemic thrombolysis is advised by the BTS and should be considered in peri-arrest situations based on clinical ground alone. Table 1 (12) includes the risk stratification as highlighted.
Acknowledgments
I would like to take this opportunity to thank our patients for allowing us to use their cases to further our knowledge.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Informed consent was obtained from the patient for publication of this Case report.
References
- Oger E. Incidence of venous thromboembolism: a community-based study in Western France. EPI-GETBP Study Group. Groupe d'Etude de la Thrombose de Bretagne Occidentale. Thromb Haemost. 2000;83:657-60. [Crossref] [PubMed]
- Radcliffe Cardiology. Table 2: Contraindications To Thrombolytic Therapy. Available online: https://www.radcliffecardiology.com/image-gallery/table-2-contraindications-thrombolytic-therapy
- Mehta NJ, Jani K, Khan IA. Clinical usefulness and prognostic value of elevated cardiac troponin I levels in acute pulmonary embolism. Am Heart J 2003;145:821-5. [Crossref] [PubMed]
- Malekan R, Saunders PC, Yu CJ, et al. Peripheral extracorporeal membrane oxygenation: comprehensive therapy for high risk massive pulmonary embolism. Ann Thorac Surg 2012;94:104-8. [Crossref] [PubMed]
- Aymard T, Kadner A, Widmer A, et al. Massive pulmonary embolism: surgical embolectomy versus thrombolytic therapy--should surgical indications be revisited? Eur J Cardiothorac Surg 2013;43:90-4; discussion 94. [Crossref] [PubMed]
- Neely RC, Byrne JG, Gosev I, et al. Surgical Embolectomy for Acute Massive and Submassive Pulmonary Embolism in a Series of 115 Patients. Ann Thorac Surg 2015;100:1245-51; discussion 1251-2. [Crossref] [PubMed]
- Konstantinides S, Geibel A, Heusel G, et al. Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism. N Engl J Med 2002;347:1143-50. [Crossref] [PubMed]
- Marti C, John G, Konstantinides S, et al. Systemic thrombolytic therapy for acute pulmonary embolism: a systematic review and meta-analysis. Eur Heart J 2015;36:605-14. [Crossref] [PubMed]
- Chatterjee S, Chakraborty A, Weinberg I, et al. Thrombolysis for pulmonary embolism and risk of all-cause mortality, major bleeding, and intracranial hemorrhage: a meta-analysis. JAMA 2014;311:2414-21. [Crossref] [PubMed]
- Meyer G, Vicaut E, Danays T, et al. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med 2014;370:1402-11. [Crossref] [PubMed]
- British Thoracic Society Standards of Care Committee Pulmonary Embolism Guideline Development Group. British Thoracic Society guidelines for the management of suspected acute pulmonary embolism. Thorax 2003;58:470-83. [Crossref] [PubMed]
- Malik S, Bhardwaj A, Eisen M, et al. Advanced Management Options for Massive and Submassive Pulmonary Embolism. US Cardiol Rev 2016;10:30-5. [Crossref]
Cite this article as: Chowdhury D. Consideration for thrombolysis for significant pulmonary embolism in haemodynamically stable patients—is it time for a rethink? J Emerg Crit Care Med 2019;3:53.