Lessons learnt from handling an outbreak of gastroenteritis from the emergency department perspective
Introduction
The patterns and epidemiology of foodborne disease have been changing over the years. Still a major cause of mortality amongst developing nations (1), developed countries are seeing an increase in prevalence of foodborne diseases due to changes in eating habits, increased consumption of commercially prepared food and centralized food production (2).
Singapore is a densely populated city in South-east Asia. Despite being known for its cleanliness and standards of hygiene, it is no stranger to food-borne outbreaks. In particular, Salmonella species have often been implicated in such outbreaks. These include an outbreak in 2007 linked to consumption of cream cakes (3), an outbreak in 2006 linked to canteen food (4), as well as an outbreak in a military camp in 2007 (5). The Singapore Institute of Food Science and Technology noted an “alarming increase in non-typhoidal salmonellosis” from 2002–2012 (6) and the Ministry of Health made salmonellosis a mandatory notifiable disease in Singapore under the Infectious Disease Act (7).
The threat of bioterrorism is also concerning in this day and age. Whilst a major food-borne bioterrorism attack paralleling the Rajneesh incident many years ago has not been seen (8), bio-terrorism in the form of the post 9–11 anthrax scare has kept medical practitioners worldwide on a heightened state of readiness (9).
Singapore is a small, highly connected and densely populated country, where any bioterrorism attack would spread quickly and be catastrophic. The doctors in the ED are the frontline in combating such events and have a huge responsibility in identifying the red-flags that suggest a major event, at the same time maintaining pragmatic control over the already scarce healthcare resources.
Case scenario
In August 2008, a serious gastroenteritis outbreak occurred amongst foreign workers working in a construction site in Singapore. A total of 76 patients presented over four days with diarrhea, vomiting and abdominal pain. A review of the dietary history as taken by the ED physician attending to them revealed that they all ate at the same canteen on the day of symptom onset. They were subsequently found ill by their dormitory supervisor and sent in by the busloads to the ED of a tertiary academic medical hospital in Singapore that was about two kilometers from the dormitory.
This event was one of the most serious outbreaks of gastroenteritis reported in Singapore and was initially managed as a potential bioterrorism attack. Managing the outbreak revealed the challenges involved in forming a pragmatic response to a situation that could potentially be a bioterrorism attack in the guise of a simple illness. The purpose of this study is to identify the learning points that can be gleaned from such an event. This could aid in formulating future protocols for such future events.
Methods
The study was done in a tertiary academic medical center with 1,597 acute beds. The ED of the study has an annual workload of roughly 146,899 patient visits (10).
A retrospective chart review was done, and all visits to the emergency department from two days before the outbreak till two weeks after were screened. In addition to all the patients brought in on the same busloads from the same location, all other patients with presenting complaints related to gastroenteritis (vomiting, abdominal pain, diarrhea, nausea, fever) were screened to determine if they presented from a similar location or had a similar dietary history. Patients who presented from a different location or had a different dietary history were excluded. Of the patients identified, data on ED arrival time, patient’s addresses, dietary history, symptoms, signs, treatment given, disposition and any microbiological tests done were collected from the patient’s medical chart. All data were collected onto a standardized data collection form and a random sampling of 10% of the patients were chosen for performance monitoring by another study member.
Written informed consent was not necessary because no patient data has been included in the manuscript.
A descriptive analysis was performed using the statistical package in Microsoft Excel. Inpatient records of the patients admitted were also reviewed. The medical personnel involved in the outbreak were also interviewed with regard as to their decisions made and thought processes concerning the outbreak. This study was granted approval by the Singhealth Centralised Institutional Review Board (CIRB Ref: 2018/2015).
Results
Patient presentation and initial ED response
The outbreak presented itself at the ED without any prior warning, with the first batch of 27 patients arriving by bus at 2,100 hours. Due to concerns of this incident being a deliberate event and not a simple gastroenteritis outbreak, immediate measures were put in place for the patients to be located separately and to be seen by two designated doctors under the supervision of a senior doctor. An observation ward was partitioned off for this purpose and cohort nursing was also implemented. A doctor not on duty was informed and put on standby in case the existing staff could not handle the workload in the department.
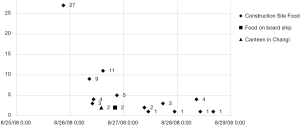
Subsequently, several batches of patients identified to be from the same cluster continued to come into the ED over the next three days, the numbers of each batch ranging from 1–9 (Figure 1). These patients were similarly seen separately by a pre-designated group of doctors at predefined area as stated previously. All doctors observed standard universal precautions and paid careful attention to hand hygiene. All equipment and waste (vomitus & stool) were disposed of in biohazard bags.
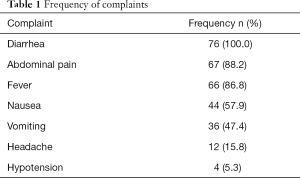
The most frequent complaint was that of diarrhea (76, 100%), followed by abdominal pain (67, 88.1%) (Table 1). The initial possibility of a bioterrorism attack was considered on the night of the outbreak. A standard treatment protocol was drawn up to include symptomatic treatment, antibiotics, observation and cohort nursing. The pathogen causing the gastroenteritis was not identified initially.
Full table
All the patients received symptomatic treatment in the form of intravenous fluid administration/anti-emetics, and 12 patients (15.8%) received antibiotics based on severity of clinical symptoms/signs. The antibiotic decided upon was ciprofloxacin and subsequently by the end of the first night of the outbreak, a treatment protocol that suggested the usage of ciprofloxacin was suggested. Subsequently, 35 of the remaining 49 patients (71.4%) received the empiric antibiotics.
Incident reporting and infectious disease input
The incident was immediately reported to the Singapore Ministry of Health (MOH). Review of patient’s charts suggested a particular cookhouse as the source of the outbreak and this was reported for further investigations. This was because of the common factor of all patients eating the same dinner at that cookhouse on the night of the outbreak.
The inpatient infectious disease team was also informed and consulted on the same night. A team of infectious disease doctors was allocated to round on all the cohort patients being observed in the ED, to aid in determining need for further interventions. This reduced the strain on the ED staffing.
Microbiological testing and antibiotic choice
All patients received basic blood investigations including a renal panel and a full blood count. Microbiological studies were also conducted on patients who were admitted to the ward, and subsequently on all patients who had a repeat ED attendance. The inpatient infectious disease team suggested these microbiological studies, and subsequently followed up the patients after the incident.
The decision for usage of ciprofloxacin as antibiotic cover was made empirically. This was taking into consideration common causes of gastroenteritis.
Microbiological confirmation and disposition
A total of 10 patients (13.2%) were investigated microbiologically with a total of 2 stool cultures being positive for Salmonella Enteritidis sensitive to ciprofloxacin.
A pragmatic approach was taken in order to prevent unneeded admissions. As mentioned, an inpatient infectious disease team was allocated to round the patients in the ED to aid in determining if patients needed further interventions. A total of two patients (2.63%) were admitted immediately due to abnormal vital signs. five patients (6.58%) were admitted after an 8-hour period of observation, as symptoms were not improving. Lastly, a total of 24 patients (30.2%) were discharged after observation and 45 (59.2%) were discharged after being seen.
Special cases
It must be noted that amongst the main cluster of patients presenting from the same address and workplace, one particular patient that was admitted for persistent abdominal pain was subsequently diagnosed with appendicitis and underwent an appendectomy the next day.
There were also two other small groups of patients that had presentations of gastroenteritis—three patients from a separate factory in the east of Singapore as well as two sailors from a ship docking in Singapore. These patients were treated initially as being from the same outbreak.
Discussion
In this era of densely populated cities and changing patterns of diseases, the mantra “hope for the best, prepare for the worst” is a good one to have with faced with uncertain scenarios. While our scenario turned out to be a gastroenteritis outbreak, the initial approach and lessons gleaned from approaching it initially as a potential bioterrorism attack is important. While it is always better to be safe than sorry, a pragmatic balance has to be drawn to prevent wastage of precious resources. Several important lessons can be gleaned from the outbreak outlined above.
Guidelines to planning and response to a bioterrorism attack are available (11) and include suggestions on preparing for a disaster, precautions to prevent transmission, identification of agent based on syndrome, and subsequent empiric treatment.
According to the CDC Strategic Planning Workgroup (12), Salmonella species as well as most diarrhea illness causing organisms are Category B agents, which are second-highest priority agents that are moderately easy to disseminate.
EDs should have in place rough guidelines and protocols to activate when a bioterrorism attack is suspected. Whilst protocols might not address all possibilities and will certainly not be exhaustive, a rough framework to rely on in times of confusion and urgency will aid greatly in a smooth response.
Several features aid us in distinguishing a natural disease outbreak form a bioterrorist attack (Table 2) In particular, the following features were worrying to us: sudden presentation of large numbers, presenting at a similar stage in disease epidemiology, presentation of a disease that could be caused by a CDC Category B agent.

Full table
Our hospital responded in a timely manner with immediate cohorting of the patients in one observation ward separate from other patients. Having particular doctors and nurses taking care of the entire cohort of patients serves not only to reduce transmission of disease, but also serves to increase efficiency is identifying trends of the outbreak, potentially helping to further understand the exact problem being dealt with. Basic cohorting measures do not necessarily require a large amount of additional manpower, and there should be a low threshold before initiating this step in combating a potential bioterrorist attack.
Patient isolation is a slightly trickier issue. In this outbreak, the patients were subjected to Standard and Contact precautions, and this is appropriate for the syndrome being dealt with. Consideration as to the potential pathogen will have to be given, and accordingly the precautions escalated to droplet or even airborne precautions.
Whilst it is pragmatic to treat the patients according to each individual patient’s signs and symptoms, one has to consider the entire situation at the same time. In this case, the patients presented with signs and symptoms of gastroenteritis and this fit in with the possibility of a gastroenteritis outbreak. Each patient was assessed individually and decisions made based on each patients clinical condition. However, the possibility of other more sinister scenarios was always considered, including that of a bioterrorism attack, organophosphate poisoning, or radiation sickness. Of course, without other clues that suggest one of these, treatment would be withheld until there are more suggestive pieces of information.
It is also important to notify the relevant authorities as soon as possible, so as to facilitate public health control measures. Early investigation of the outbreak could potentially provide a clear answer as to exactly what treatment should be initiated. Delays in this could result in negative investigations and inability to determine the source of the outbreak. Equally important is early involvement of the infectious disease teams of the hospital. This will allow a continuity of care as well as reduce the strain on the ED. The infectious disease teams of our hospital helped to formulate the protocols and rounded on the patients in the mornings, greatly reducing the strain on the already busy ED.
Once the ED has a clearer grasp on what they are dealing with, a protocol on how to deal with each patient is greatly beneficial. It allows doctors to assess each patient quickly and also ensures that the relevant information is collected, and the appropriate treatment given. In order to achieve this, early notification to the authorities and involvement of other specialists is needed. In our experience, the protocol aided physicians in their decision making process for admission/observation/discharge, as well as their choice of empirical antibiotics. The choice of antibiotics was based on local data on the common gastroenteritis pathogens and sensitivities, as well as a suspicion of suspected food-borne bioterrorism.
Another aspect to consider is that bioterrorism tends to have sustained course due to pathogen incubation period, and the patients could present over many days after the initial event as the pathogen continues its spread in the community. This could be heavily draining on any ED’s resources, especially if drastic measures have to be kept up for days. A pragmatic approach focusing on cohorting and protocol based care is recommended.
Last but not least, as evidenced by the patient found to have an inflamed appendix, the eventual responsibility is on every clinician to remember that each patient is still an individual with unique needs and backgrounds. Therein lies the challenge in being on the frontline of any disease outbreak, whether bioterrorism related or not.
The biggest limitations to our study arise from the fact that the outbreak occurred many years ago. As such, physicians who dealt with the outbreak would be prone to recall bias, possibly painting a more ideal response to the scenario. We are also reliant on old records for all descriptive analysis of the event, which is prone to errors in documentation. Nonetheless, we believe the description of the event and subsequent evaluation of the department’s response offers precious lessons to be learnt. Personnel involved in data collection were also not blinded. However this is unlikely to affect our study results, as it is a descriptive study of an event.
Conclusions
Frontline physicians in the ED need to maintain constant vigilance for potential bioterrorism attacks that can arrive in the guise of other illnesses or minor disease outbreaks. Initiating simple cohorting measures early is worthwhile and not very resource intensive. Early involvement of inpatient specialists and notification of the authorities will aid in formulating clearer long term plans and protocols which will further reduce the strain placed on the ED.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Approved by Singhealth Centralised Institutional Review Board (CIRB Ref: 2018/2015). Need for informed consent was waived as most of the patients no longer reside in Singapore and no identifiable personal data was collected. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and its later amendments.
References
- Scott E. Food safety and foodborne disease in 21st century homes. Can J Infect Dis 2003;14:277-80. [Crossref] [PubMed]
- McCabe-Sellers BJ, Beattie SE. Food safety: emerging trends in foodborne illness surveillance and prevention. J Am Diet Assoc 2004;104:1708-17. [Crossref] [PubMed]
- Ministry of Health, Singapore. Epidemiological News Bulletin 2008. Available online: https://www.moh.gov.sg/content/dam/moh_web/Statistics/Epidemiological_News_Bulletin/2008/ENB01Q_08.pdf. Published 2008. Accessed February 2015
- Ministry of Health, Singapore. Communicable Diseases Surveillance in Singapore 2006. Available online: https://www.moh.gov.sg/content/dam/moh_web/Publications/Reports/2007/2/Special%20Feature (4).pdf. Published 2006. Accessed February 2015
- Lee VJ, Ong AES, Auw M. An outbreak of Salmonella gastrointestinal illness in a military camp. Ann Acad Med Singapore 2009;38:207-11. [PubMed]
- Kondakci T, Hyun GY. Overview of foodborne outbreaks in last decade in Singapore: Alarming increase in nontyphoidal salmonellosis. Food Beverage Asia 2012;12:42-5.
- Ministry of Health, Singapore. Infectious Disease Act. Available online: https://www.moh.gov.sg/content/moh_web/home/legislation/legislation_and_guidelines/infectious_diseasesact.html. Published 2007. Accessed February 2015.
- 1984 Rajneeshee bioterror attack. Wikipedia. Available online: https://en.wikipedia.org/wiki/1984_Rajneeshee_bioterror_attack. Accessed February 2015
- Wills B, Leikin J, Rhee J, et al. Analysis of suspicious powders following the post 9/11 anthrax scare. J Med Toxicol 2008;4:93-5. [Crossref] [PubMed]
- Quick Facts. Singapore General Hospital Website. Available online: http://www.sgh.com.sg/about-us/more-about-sgh/pages/quickfacts.aspx. Accessed February 2015.
- Centers for Disease Control and Prevention. Bioterrorism Readiness Plan: A Template for Healthcare Facilities. Available online: http:// . Published 1999. Accessed February 2015http://emergency.cdc.gov/bioterrorism/pdf/13apr99apic-cdcbioterrorism.pdf
- Centers for Disease Control and Prevention. Biological and Chemical Terrorism: Strategic Plan for Preparedness and Response. Recommendations of the CDC Strategic Planning Workgroup. Available online: http://www.cdc.gov/mmwR/PDF/rr/rr4904.pdf. Published 2000. Accessed February 2015
Cite this article as: Liu Z, Ponampalam R. Lessons learnt from handling an outbreak of gastroenteritis from the emergency department perspective. J Emerg Crit Care Med 2020;4:9.