
Haemothorax following removal of an internal jugular central venous catheter
A 52-year-old lady was admitted to the intensive care unit (ICU) with decompensated dilated cardiomyopathy requiring a Dobutamine infusion via a right internal jugular central venous catheter (CVC).
Her CVC was removed once her cardiac function stabilised. Over the next hour, she reported light-headedness, neck and shoulder pain and her blood pressure dropped from 96/61 to 72/43 mmHg. Her haemoglobin dropped from 112 to 77 g/L over the next four hours. Her coagulation profile was normal. An ultrasound showed no evidence of a neck haematoma.
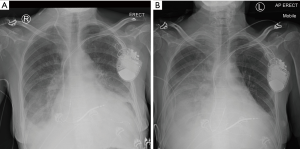
Chest X-rays taken pre-CVC removal (Figure 1A) and post-CVC removal (Figure 1B) are shown below, with the latter showing a new right pleural effusion. A large haemothorax was later confirmed with lung ultrasound and pleural drainage of 800 mL of blood-stained fluid.
Her condition stabilised following transfusion of 2 units of packed red blood cells and no further intervention was required. A subsequent computed tomography (CT) angiogram showed no carotid artery injury.
Haemothorax following removal of a CVC is a rare but recognised complication (1,2). There are no documented case reports of this complication following removal of an internal jugular vein CVC. The low insertion position of this catheter in the neck likely contributed to this patient’s elevated risk. Pleural injury during catheterisation, erosion of the vessel wall, accidental arterial puncture and repeated attempts at cannulation are all risk factors for this complication (3). Hypotension temporally associated with the removal of a CVC should raise the possibility of a haemothorax in this patient group.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm.2020.03.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Approval was obtained from the ethics committee of The Alfred Hospital, Melbourne, Australia.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Collini A, Nepi S, Ruggieri G, et al. Massive hemothorax after removal of subclavian vein catheter: a very unusual complication. Crit Care Med 2002;30:697-8. [Crossref] [PubMed]
- Lee HK, Hong SW, Kim GJ, et al. Massive hemothorax immediately after removal of central venous catheter -A case report-. Korean J Anesthesiol 2013;65:77-9. [Crossref] [PubMed]
- Polderman KH, Girbes AJ. Central venous catheter use. Part 1: mechanical complications. Intensive Care Med 2002;28:1-17. [Crossref] [PubMed]
Cite this article as: Costa-Pinto R, Pearson J, Orosz J, Udy A. Haemothorax following removal of an internal jugular central venous catheter. J Emerg Crit Care Med 2020;4:28.


