Outcomes of patients requiring prolonged mechanical ventilation in Singapore
Introduction
Advances in medical care have enabled more patients in the intensive care unit (ICU) to survive the acute stage of critical illness. However, some have persistent organ failures and remain dependent on mechanical ventilator. According to the National Association for Medical Direction of Respiratory Care (NAMDRC) Consensus Conference in 2005, prolonged mechanical ventilation (PMV) was defined as the use of mechanical ventilator for at least 6 h/day for 21 days or more (1). Prior studies have estimated that approximately 3% to 7% of ICU patients ended up requiring PMV (1). This number is predicted to increase over the years as a result of increasingly complex patient profiles: advanced age, multiple comorbidities and less physiological reserves (2).
It is important to understand the outcomes and prognostic factors of these patients as the amount of healthcare resources and medical expenses they consume is disproportionate (3). It also allows physicians to provide patients and families with realistic expectations of outcomes, which helps to facilitate resource planning, determine goals of care and end of life planning.
Most studies on patients requiring PMV were done in Western countries/regions (4-6), with a few done in Asia, mainly Taiwan and Korea (7-10). To date, there has not been any prior publication of PMV outcomes in Singapore or in South East Asia.
We aim to describe the clinical characteristics of patients requiring PMV in Singapore, examine the survival outcomes and identify important prognostic factors that predict mortality in these patients. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jeccm-20-61).
Methods
Study design and patients
This was a retrospective cohort study conducted at Tan Tock Seng Hospital, Singapore, which is a university-affiliated tertiary care hospital with a 12-bed medical ICU at the time of data collection. In addition, there are separate 8-bed coronary care unit, 8-bed surgical ICU and 12-bed neurology/neurosurgical ICU. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013), and ethics approval for the use of clinical data was obtained from Singapore National Healthcare Group Domain Specific Review Board (NHG DSRB reference number 2016/0170). Informed consent for this retrospective study was waived. All adult patients (≥18 years old) admitted to medical ICU between 2012 and 2015 who required PMV (invasive and non-invasive mechanical ventilation for ≥21 days) were included in the study. Exclusion criteria were patients with pre-existing chronic mechanical ventilation, chronic neuromuscular disease, or patients who had tracheostomy for reasons other than acute respiratory failure (e.g. head and neck malignancy). For patients with repeated prolonged ICU admissions, we recorded and analysed only data from the initial ICU admission.
The following data were collected from the electronic medical record system: age, gender, race, comorbidities, premorbid functional status, admission source, primary reason for ICU admission, Acute Physiology and Chronic Health Evaluation II (APACHE II) score on day 1 of ICU admission, lab results, duration of mechanical ventilation, length of stay in the ICU and hospital, tracheostomy rate, ICU and hospital mortality, 180-day mortality, and 1-year mortality. For patients who survived till hospital discharge, we also obtained information about their discharge destination and functional status at discharge. These patients were followed up for 1 year from ICU admission date.
The primary outcome was 180-day mortality. Secondary outcomes were ICU mortality, in-hospital mortality, 1-year mortality, factors that predict mortality, and placement and functional status at discharge.
Statistical analysis
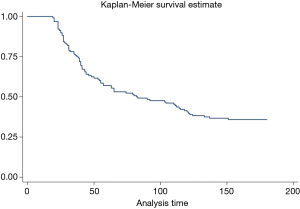
Statistical analyses were performed using the SPSS version 20 (SPSS Inc., Chicago, IL, USA) with complete case analysis. Survivors were defined as patients who survived for more than 180 days after ICU admission. Non-survivors were patients who died within 180 days. Differences between survivors and non-survivors were explored using the chi-square and Fisher’s exact test for categorical variables; and student t-test and Mann-Whitney U test for continuous variables. Kaplan-Meier curves were drawn to show median survival time of the patient cohort. Cox proportional hazard model was performed to rule out the prognostic factors for 180-days mortality. Event was defined as 180-day mortality; missing data and loss to follow up were otherwise censored. Variables with P value less than 0.200 in the univariate analysis were included into the multivariate model for variable selection. Multicollinearity, interaction term and assumptions were checked for the final model, with P value less than 0.05 considered as statistically significant.
Results
Clinical characteristics of patients
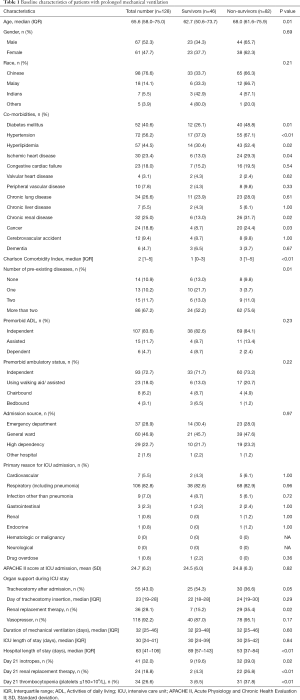
During the study period, there were a total of 128 patients requiring PMV. Median [interquartile range, IQR] age was 66 [58–75] years old. Sixty-seven (52.3%) were males. The majority of patients were Chinese (n=98, 76.6%), reflecting the general demographics of Singapore population. The most common comorbidities were hypertension (n=72, 56.2%), hyperlipidemia (n=57, 44.5%) and diabetes mellitus (n=52, 40.6%), with a median (IQR) Charlson Comorbidity Index of 2 [1–5]. Mean APACHE II score was 24.7±6.2. The primary reason for ICU admission was predominantly respiratory cause (including pneumonia) (n=106, 82.8%), followed by other infections (n=9, 7.0%) and cardiovascular cause (n=7, 5.5%). Fifty-five patients (43.0%) had tracheostomy placement after admission; and the median (IQR) period from ICU admission to tracheostomy insertion was 23 [19–28] days. Median [IQR] duration of mechanical ventilation was 32 [25–46] days; ICU length of stay was 30 [24–41] days; and hospital length of stay was 63 [41–106] days (Table 1).
Full table
Primary outcome: 180-day mortality
Out of 128 patients, there were 46 survivors and 82 non-survivors, translating to a 180-day mortality rate of 64.1%. Baseline characteristics of the two groups are significantly different. Non-survivors were older, with a median [IQR] age of 68 [62–76] years old compared to 63 [51–74] years old in survivors. Non-survivors also had more pre-existing diseases, and higher Charlson Comorbidity Index of 3 [1–5] compared to 1 [0–3] in survivors. In particular, non-survivors had more of the following co-morbidities: hypertension, hyperlipidemia, diabetes mellitus, ischemic heart disease, chronic renal disease and cancer. There was no difference in the APACHE II score at ICU admission between non-survivors and survivors.
Non-survivors had fewer tracheostomy placement (n=30, 36.6%) compared to survivors (n=25, 54.3%). Although duration of mechanical ventilation and ICU length of stay are similar, non-survivors have significantly shorter hospital length of stay, median [IQR] of 53 [37–84] days compared to 89 [57–143] days in survivors. Non-survivors also had significantly more patients with inotropic support, renal replacement therapy and thrombocytopenia at day 21 of ICU admission (Table 1).
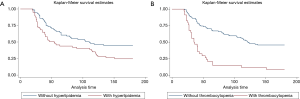
Kaplan Meier curve showed a median survival time of 82 days in the patient cohort (Figure 1).
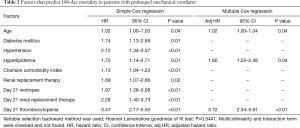
Predictors of mortality
In the multivariate analysis using Cox proportional hazards regression, three factors predict 180-day mortality in patients with PMV: (I) age; (II) comorbidity of hyperlipidemia; (III) day 21 thrombocytopenia (platelets ≤150×109/L), with a hazard ratio of 1.02 [1.00–1.04], 1.60 [1.03–2.49] and 3.72 [2.34–5.91] respectively (Table 2, Figure 2).
Full table
Other secondary outcomes
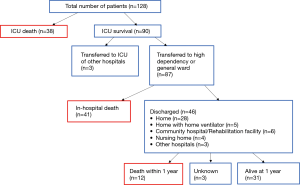
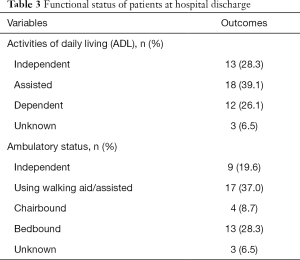
ICU mortality rate was 29.7%, in-hospital mortality rate was 61.7%, and 1-year mortality rate was 71.1% (Figure 3).
Of the 46 patients who survived hospital admission and were discharged, 28 (60.9%) went home, 6 (13.0%) were transferred to community hospital or rehabilitation facility, 4 (8.7%) to nursing home, 3 (6.5%) to other hospitals and 5 (10.9%) required long term home mechanical ventilation. Twelve (26.1%) were dependent in activities of daily living and 13 (28.3%) were bedbound at discharge (Figure 3 and Table 3).
Full table
Discussion
Patients requiring PMV represent an emerging challenge for the healthcare system: they embody a distinct cohort of ICU patients with high mortality and high burden of care. In our study, the 180-day mortality was 64.1%. This was comparable to the study done by Kim et al. in South Korea, which reported a 180-day mortality of 58.8% (10). In a large population-based study in Taiwan by Lu et al., the 3-month and 1-year mortality was 48.6% and 68.1% respectively (7). On the other hand, patients in respiratory care centres in Taiwan—a subacute stage for weaning training, had a lower in-hospital mortality of 17.6% in a study by Lai et al. (8) and 16.6% by Huang (9).
In the West, there were more publications on PMV, with the reported in-hospital mortality ranging from 28.0% to 40.3%; and 1-year mortality ranging from 48.0% to 59.0% (5,6,11). Our study found an in-hospital mortality of 61.7%, and 1-year mortality of 71.1%, which were higher than what was reported in the literature. These differences in mortality rate can be explained by: heterogeneity of the study setting and study population; variation in healthcare systems and practices; and different definitions of PMV in the literature.
After the acute phase of critical illness in ICU, some patients survive but remain dependent on mechanical ventilation, resulting in a syndrome of persistent organ dysfunction, profound weakness and extreme symptom burden, also known as chronic critical illness (12). Traditionally, these patients are managed in the acute hospitals. However, over the years, their care has evolved to include specialised weaning unit in the subacute setting, for example the long-term acute care hospitals in United States, and respiratory care centres in Taiwan (8,9,13). In Singapore, there is no dedicated step-down facility for patients with PMV. These patients remain in the acute hospital, usually in the ICU; or high dependency if able to use portable mechanical ventilator or non-invasive ventilation. Those who fail weaning end up with protracted ICU and hospital stay until one of the following outcomes: (I) successful weaning; (II) death, usually from the underlying disease process or complications of PMV (the most common inpatient cause of death in our study cohort was pneumonia); or (III) discharge home with mechanical ventilation. Although home mechanical ventilation is an option, there were only 5 patients in our study cohort who were discharged home with mechanical ventilation. This was largely due to the lack of dedicated carer or social support at home, in addition to the financial burden involved from the loss of income and the need to hire help to assist with the care of these patients (14). These factors can explain our long ICU and hospital length of stay, and indirectly the higher in-hospital mortality rate. As previous published single centre and regional studies on PMV have been conducted at different settings (e.g., ICUs in acute care hospitals, weaning units in acute care hospitals and post-acute care hospitals) with heterogeneous study population and diverse healthcare systems, it makes direct comparison of outcomes challenging.
Previous studies have also used different definitions of PMV: ≥96 hours, ≥14 days, ≥21 days or >29 days of mechanical ventilation; which can account for the differences in mortality outcomes reported in the literature (1). The most commonly used definition was the NAMDRC consensus of mechanical ventilation use for at least 6 hours/day for 21 days or more (1). In Taiwan and United States, this criterion is applied to step patients down to lower level of care (13). Some authors suggest that the number of consecutive days may be an arbitrary marker (13), and may not the best criteria to identify transition of acute to PMV, or in a broader sense transition of acute to a more chronic phase of critical illness—which has greater clinical implication. This area was explored by Iwashyna et al. who introduced an intriguing concept of persistent critical illness, defined as a time point during critical illness beyond which acute diagnoses and physiologic disturbances at ICU presentation cease to predict mortality outcome more accurately than antecedent patient characteristics—i.e., the patients’ reason for being in ICU is now more related to their ongoing critical illness (be it due to endocrine dysregulation, unresolved inflammation or hospital-acquired complications) than their original reason for ICU admission (15). Using large population database from Australia and New Zealand, they found this transition point to be at day 10 (15). Subsequent studies in Canada found the transition point to be at day 9 (16); in United Kingdom, it was day 5 to 8 (17); and in United States among patients with sepsis, it ranged from day 6 to 27 (18). Regardless of which time points, patients with persistent critical illness have been shown to use disproportionate amount of ICU resources, and had generally worse outcomes. In a way, the findings in our study concurred with the notion of persistent critical illness: there was no difference between survivors and non-survivors in their APACHE II score at ICU admission; in fact, baseline demographics and comorbidities appeared more prognostically important in determining survival outcomes.
Another unique cultural difference in Asian population is societal view on filial piety and the heavy involvement of family members in decision making. Unlike Western countries in which patient autonomy is emphasized, in Asia, an individual is often regarded as a smaller self within a larger self, specifically the family; hence decisions are often made from the family’s perspective (19). To complicate matters further, death and dying is viewed as a taboo subject in many Asian cultures and not discussed opening, resulting in a lack of advanced directives to guide decision making (20). This unawareness of patient’s preferences, together with a strong sense of reverent responsibility towards family members, may lead to continuation of aggressive life support, and inadvertently creating patients who survive acute critical illness but with persistent organ dysfunction and unable to wean off mechanical ventilator.
There were some interesting findings in our study. We found that non-survivors had fewer tracheostomy placement and a shorter hospital length of stay. Both survivors and non-survivors had tracheostomy inserted late into their ICU admission, with a median of >21 days. This may reflect difficulties in achieving consensus between physicians and families of patients. In our study, the duration of mechanical ventilation (invasive and non-invasive) was longer than ICU length of stay. This is because some patients were transferred to high dependency while undergoing weaning (e.g., those who were extubated to non-invasive ventilation).
In terms of predictors of mortality, we found similar predictors of poor outcome as the ProVent score developed by Carson et al. in 2008 (21). Specifically, in the multivariate analysis, age and day 21 thrombocytopenia were found to be statistically significant. Requirement for inotropes and renal replacement therapy at day 21 were also significant in the univariate analysis, but not in the multivariate analysis. The reason for this could be related to sample size; or difference in outcome measures: 180-day mortality in our study versus 1-year mortality in the ProVent score. However, in another study by Kim et al. in South Korea which looks at 180-day mortality, thrombocytopenia and requirement for vasopressors at day 21 were associated with higher mortality (10). Other prognostic factors discovered by Lu et al. in Taiwan include neoplasms, renal failure, shock, septicemia and non-alcoholic liver disease (7). Interestingly, our study also found hyperlipidemia as an independent predictor of mortality. We postulate that hyperlipidemia is likely a reflection of underlying cardiovascular burden, which can explain the higher 180-day mortality, nevertheless this requires further studies.
A major strength of this study is the inclusion of discharge destination and functional status at discharge. They are of utmost concerns to physicians, patients and families. They are also of great interest to policy makers. Knowing the level of care required after PMV can assist in discharge planning and help manage patients’ and families’ expectations.
Our study had several limitations. First, it was a single centre, retrospective cohort study. It represented our centre’s organisation and care process, and may not be generalisable. Second, our sample size was relatively small compared to other published cohorts. Hence important prognostic factors with smaller effects may not be apparent in the multivariate analysis. Third, we did not examine the long-term quality of life, cognition and mental health effects among survivors, which are important aspects in chronic critical illness. Forth, we did not evaluate the healthcare cost incurred by these patients with PMV.
In conclusion, patients requiring PMV represent a distinct cohort of ICU patients with high mortality and high burden of care. This number is expected to rise further with an aging population. As they consume disproportionate amount of medical resources, it will place further strain on the healthcare system. The result of this study is an important first step to create awareness about the extent of PMV in Singapore, including survival outcomes and prognostic factors. While ICU setting is apt at managing critically ill patients in the acute stage, they may lack the necessary focus and organisational structure to care for patients with prolonged weaning failure. Perhaps the role of a dedicated weaning unit for these patients will be more suited to create a bridge to home environment, and at the same time relieve the pressure on scarce ICU beds. There is no doubt that further prospective studies on PMV are needed to address the above questions to enable better care for these patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jeccm-20-61
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jeccm-20-61
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-61). The authors have no conflicts of interest to declare.
Ethics Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013), and ethics approval for the use of clinical data was obtained from Singapore National Healthcare Group Domain Specific Review Board (NHG DSRB reference number 2016/0170). Informed consent for this retrospective study was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- MacIntyre NR, Epstein SK, Carson S, et al. Management of patients requiring prolonged mechanical ventilation: report of a NAMDRC consensus conference. Chest 2005;128:3937-54. [Crossref] [PubMed]
- Carson SS, Bach PB. The epidemiology and costs of chronic critical illness. Crit Care Clin 2002;18:461-76. [Crossref] [PubMed]
- Hill AD, Fowler RA, Burns KE, et al. Long-Term Outcomes and Health Care Utilization after Prolonged Mechanical Ventilation. Ann Am Thorac Soc 2017;14:355-62. [Crossref] [PubMed]
- Nelson JE, Cox CE, Hope AA, et al. Chronic critical illness. Am J Respir Crit Care Med 2010;182:446-54. [Crossref] [PubMed]
- Carson SS, Kahn JM, Hough CL, et al. A multicenter mortality prediction model for patients receiving prolonged mechanical ventilation. Crit Care Med 2012;40:1171-6. [Crossref] [PubMed]
- Lone NI, Walsh TS. Prolonged mechanical ventilation in critically ill patients: epidemiology, outcomes and modelling the potential cost consequences of establishing a regional weaning unit. Crit Care 2011;15:R102. [Crossref] [PubMed]
- Lu HM, Chen L, Wang J, et al. Outcomes of prolonged mechanic ventilation: a discrimination model based on longitudinal health insurance and death certificate data. BMC Health Serv Res 2012;12:100. [Crossref] [PubMed]
- Lai CC, Shieh JM, Chiang SR, et al. The outcomes and prognostic factors of patients requiring prolonged mechanical ventilation. Sci Rep 2016;6:28034. [Crossref] [PubMed]
- Huang C. How prolonged mechanical ventilation is a neglected disease in chest medicine: a study of prolonged mechanical ventilation based on 6 years of experience in Taiwan. Ther Adv Respir Dis 2019;13:1753466619878552. [Crossref] [PubMed]
- Kim MH, Cho WH, Lee K, et al. Prognostic factors of patients requiring prolonged mechanical ventilation in a medical intensive care unit of Korea. Tuberc Respir Dis (Seoul) 2012;73:224-30. [Crossref] [PubMed]
- Damuth E, Mitchell JA, Bartock JL, et al. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med 2015;3:544-53. [Crossref] [PubMed]
- Maguire JM, Carson SS. Strategies to combat chronic critical illness. Curr Opin Crit Care 2013;19:480-7. [Crossref] [PubMed]
- Rose L, McGinlay M, Amin R, et al. Variation in Definition of Prolonged Mechanical Ventilation. Respir Care 2017;62:1324-32. [Crossref] [PubMed]
- Tan GP, Soon LHY, Ni B, et al. The pattern of use and survival outcomes of a dedicated adult Home Ventilation and Respiratory Support Service in Singapore: a 7-year retrospective observational cohort study. J Thorac Dis 2019;11:795-804. [Crossref] [PubMed]
- Iwashyna TJ, Hodgson CL, Pilcher D, et al. Timing of onset and burden of persistent critical illness in Australia and New Zealand: A retrospective, population-based, observational study. Lancet Respir Med 2016;4:566-73. [Crossref] [PubMed]
- Bagshaw SM, Stelfox HT, Iwashyna TJ, et al. Timing of onset of persistent critical illness: A multi-centre retrospective cohort study. Intensive Care Med 2018;44:2134-44. [Crossref] [PubMed]
- Shaw M, Viglianti EM, McPeake J, et al. Timing of onset, burden, and postdischarge mortality of persistent critical illness in Scotland, 2005-2014: A retrospective, population-based, observational study. Crit Care Explor 2020;2:e0102. [Crossref] [PubMed]
- Zhang Z, Ho KM, Gu H, et al. Defining persistent critical illness based on growth trajectories in patients with sepsis. Crit Care 2020;24:57. [Crossref] [PubMed]
- Tai MC. Western or Eastern principles in globalized bioethics? An Asian perspective view. Tzu Chi Medical Journal 2013;25:64-67. [Crossref]
- Koh M, Hwee PC. End-of-life care in the intensive care unit: How Asia differs from the West. JAMA Intern Med 2015;175:371-2. [Crossref] [PubMed]
- Carson SS, Garrett J, Hanson LC, et al. A prognostic model for one-year mortality in patients requiring prolonged mechanical ventilation. Crit Care Med 2008;36:2061-9. [Crossref] [PubMed]
Cite this article as: Ho S, Lim CJ, Puah SH, Lew SJW. Outcomes of patients requiring prolonged mechanical ventilation in Singapore. J Emerg Crit Care Med 2020;4:32.