
Factors associated with mortality among Asian patients diagnosed with acute pulmonary embolism in the Emergency Department
Introduction
Acute pulmonary embolism (PE) is a potentially life-threatening condition that carries a high risk of morbidity and mortality (1). A recent observational study in Canada has estimated the 30-day and 1-year mortality rates from this disease to be 3.9% and 12.9% respectively (2). A systematic review of the global disease burden of thrombosis has also found venous thromboembolism, a closely-linked precursor to PE, to be one of the leading sources of disability-adjusted life years lost globally (1).
While early diagnosis and management have been shown to improve survival rates, diagnosis of the disease is notoriously difficult, particularly in the emergency department (ED) (3). The early signs and symptoms of PE are nonspecific and often overlap with those of other cardiopulmonary conditions (2). Clinical screening modalities such as the Well’s Score have also been shown to be limited in sensitivity (4). In addition, research has found differences in PE risk and mortality amongst different ethnic groups, raising concerns that current risk assessment tools, which were developed from studies done in mainly Caucasian populations, may affect risk stratification and treatment efficacy in non-Caucasian populations (5-7).
Despite its relatively low incidence in Asia, representative literature about PE among its population remains important for improving survival rates from the disease (5,6). A paper published in 2017 evaluated the clinical characteristics, risk factors and clinical outcomes of hospitalised patients diagnosed with acute PE in Singapore (8). Another local paper proposed a new model of risk stratification in comparison to other clinical prediction tools such as Pulmonary Embolism Severity Index (PESI) (9).
The aim of our study was to (I) describe the profile of patients diagnosed with acute PE in the ED of a tertiary hospital and (II) examine patient and management factors associated with 30-day mortality among these patients.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jeccm-20-96).
Methods
Setting
This was a retrospective observational study of patients conducted at the ED of Changi General Hospital, a tertiary healthcare institution in Singapore. Patients 21 years of age and older who presented to the ED between 1st January 2016 and 31st December 2017 with an ED diagnosis of acute PE were included in the study. Patients with known diagnosis of PE on active treatment and patients who arrived at the ED in a state of cardiopulmonary arrest with no subsequent return of spontaneous circulation were excluded from the study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics review committee (CIRB 2018/2260) and individual consent for this retrospective analysis was waived.
Study design
The electronic medical records were reviewed and relevant information pertaining to demographics, clinical presentation, investigations, management, disposition and outcomes were extracted. The extracted clinical and management factors were summarized in Table 1.
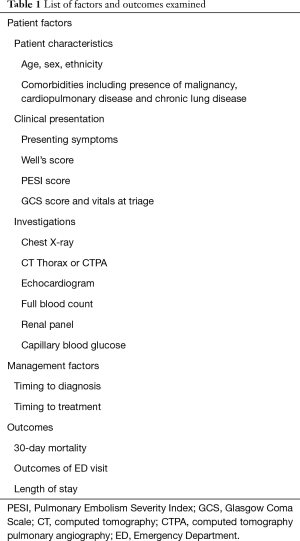
Full table
Clinical presentation
The list of variables was obtained based on literature review and included variables required in computation of PESI (8,10). The presence or absence of a recording of Well’s score in the medical records was looked for and PESI was computed retrospectively for all patients.
Investigations
Investigations and interventions done in the ED visit were populated. Both CT (computed tomography) thorax without contrast and CT pulmonary angiography (CTPA) were recorded. The clinical note was also reviewed for documentation of bedside echocardiography findings. Biochemical investigations were documented in standard units. Platelet lymphocyte ratio (PLR) and neutrophil lymphocyte ratio (NLR) was computed by platelet count or absolute neutrophil count respectively over absolute lymphocyte count.
Management
The time of presentation was taken as time patient was triaged. The time to diagnosis was the duration computed from the time of presentation to the time CT imaging was performed. The duration from time of presentation to time at which thrombolytics or anticoagulation was delivered is defined as the time to treatment.
Outcomes
The primary outcome of interest was 30-day mortality, defined as event of demise either in the ED or during inpatient stay within 30 days of ED presentation. Other variables collected were outcome of the ED visit and length of inpatient stay. Outcome of ED visit was categorized into: demise in ED, admission to Intensive Care Unit (ICU), admission to High Dependency (HD) unit, admission to general ward (GW), transfer to other hospitals and discharge against medical advice.
Statistical analysis
The data was subsequently analysed using SPSS Statistics Version 26 to correlate patient and management factors with 30-day mortality. Bivariate analysis was performed with subsequent logistic regression to determine odds ratio for all suitable variables. For categorical variables with null or complete events, comparison was done via Pearson’s chi-square instead. Statistical significance was determined by P value less than 0.05.
Results
Overall
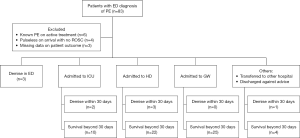
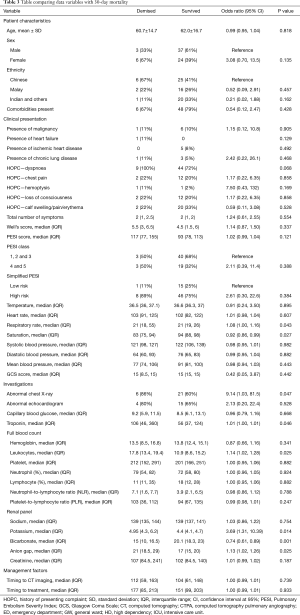
The study included a total of 70 patients (as illustrated in Figure 1) with a mean age of 61.8 (SD 16) years. Fifty-seven percent of the study population was male, 44% was of Chinese ethnicity and 77% had at least one comorbidity (Table 2). None of these patient demographics correlated significantly to 30-day mortality (Table 3).
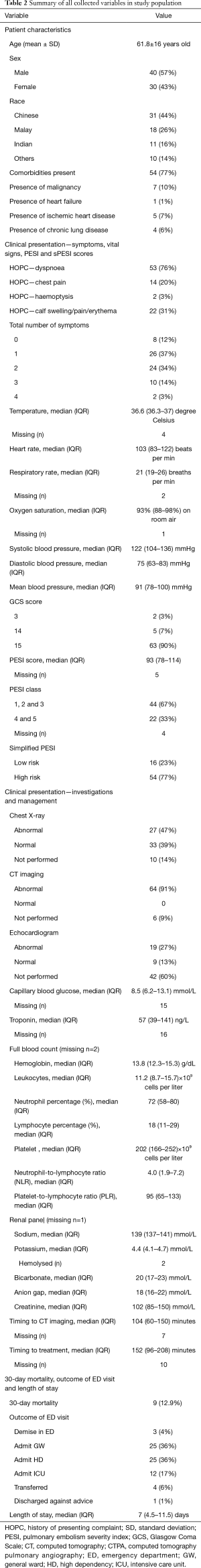
Full table
Full table
Clinical presentation
Most patients presented with at least 1–2 symptoms (71%) related to PE and/or deep vein thrombosis, with the commonest presenting symptom being dyspnoea (76%) as seen in Table 2. Out of the 14 patients presenting with loss of consciousness, 10 of them required HD or ICU care. There were only two patients (3%) who presented with hemoptysis but both had poor outcomes. They were both admitted to HD and one later demised during inpatient stay. The total number of presenting symptoms did not correlate significantly with 30-day mortality (P=0.554).
In terms of objective parameters taken at triage, the patients were mildly tachycardic (median heart rate 103 beats per minute, IQR 83–122) and tachypneic (median respiratory rate 21 breaths per minute, IQR 19–26). The median oxygen saturation reading without oxygen supplementation was 93% (IQR, 88–98%). Temperature and blood pressure readings were within normal ranges (Table 2). Majority of the patients (90%) had a GCS score of 15 at presentation. Higher respiratory rates and lower oxygen saturation levels were both significantly associated with 30-day mortality (P=0.043, P=0.027 respectively) while GCS score and blood pressure measurements at presentation did not demonstrate any correlation with 30-day mortality (Table 3).
The median PESI score was 93 (IQR, 78–114) with majority in PESI Class One, Two and Three compared to Class Four and Five (67% and 33% respectively). When applying the simplified PESI index, 54 patients (77%) were classified as high risk and the remaining 16 (23%) as low risk. None of these classifications correlated significantly with 30-day mortality (refer to Table 3). The mortality rate of PESI class 1, 2 and 3 was lower than PESI class 4 and 5 (6.9% and 13.6% respectively).
Investigations
Sixty-four patients (91%) received CT imaging which were all diagnostic of PE. Six patients (8%) had CT thorax without contrast while 58 patients (83%) had CTPA (Table 2). Chest X-rays were performed for 60 patients (86%) of which 27 (39%) showed abnormalities (such as lung opacities and pleural effusions). The presence of abnormal chest X-ray findings (found in 86% of those who demised versus 60% in survivors) were significantly associated with 30-day mortality (P=0.047, Table 3).
Amongst the 28 patients (40%) whom bedside echocardiography was performed, 19 (27%) revealed abnormal findings (Table 2). These documented abnormal findings consisted of right ventricular strain or dilatation (23%), impaired ventricular function (6%), pericardial effusion (1%) and impaired inferior vena cava collapsibility (1%).
Amongst biochemical investigations performed, five variables were found to be associated with 30-day mortality. High troponin levels (median 106 versus 56 ng/mL in survivors), high potassium levels (median 4.95 versus 4.4 mmol/L in survivors), low bicarbonate levels (median 15 versus 20.1 mmol/L in survivors), high anion gap (median 21 versus 17 in survivors) and high leucocyte counts (median 17.8×109/L versus 10.9×109/L in survivors) showed significant correlation with 30-day mortality (P=0.046, P=0.014, P=0.001, P=0.025 and P=0.025 respectively). There were no significant associations between mortality and platelet-to-lymphocyte or neutrophil-to-lymphocyte ratios (Table 3).
Management factors
The median time taken from presentation to CT imaging in our study population was 104 (IQR, 60–150) minutes whereas the median time taken from presentation to administration of therapeutics (anticoagulation or thrombolytics) was 152 (IQR, 96–208) minutes (Table 2). Shorter timing to CT imaging significantly correlated with shorter timing to therapeutics (P<0.001) as illustrated in Figure 2.
Sixty patients (86%) of the study population had treatment administered in ED (Table 2). Thrombolytics were administered to 11 patients (16%), enoxaparin was administered to 47 patients (67%) and anticoagulation was administered to 6 patients (9%). The median time from presentation to administration of the above respective treatment was 95 (IQR, 75–211), 162 (IQR, 105–205) and 216 (IQR, 137–313) minutes. Of the remaining 10 patients whom treatment was not administered in ED, one required admission to a critical care ward while the rest were admitted to GW.
The time to diagnosis and time to treatment were similar between patients who demised and survived. Patients who demised had a slightly longer median time to diagnosis and treatment (112 and 177 minutes respectively) than those who survived (104 and 151 minutes respectively). Neither correlated significantly to 30-day mortality rates (P=0.739 and P=0.933 respectively; Table 3). Further comparisons between these management factors and 30-day mortality are illustrated in the boxplots in Figure 3. Two patients who demised had no CT imaging performed but both received thrombolytics.

Outcomes
For outcome of ED visit, 3 (4%) patients died in the ED, 25 (36%) were admitted to a general ward, 25 (36%) were admitted to a HD unit and 12 (17%) were admitted to the ICU. The remaining 5 patients (7%) were either transferred to another hospital (6%) or discharged against medical advice (1%). The median length of stay was 7 days (IQR, 1–24 days). The overall 30-day mortality was 12.9% (Table 2).
Discussion
As mentioned above, the overall 30-day mortality rate reported in our study population was 12.9%. This is comparable with 30-day mortality rates from other local studies, which ranged from 5% to 13.8% (8,9). The 30-day mortality rates reported in our study stratified by PESI Classes are also consistent with published literature for the various PESI Classes (11,12).
With regards to using the PESI score and simplified PESI score (10,11,13) to predict clinical outcomes for our patient population, we found that overall, they do not demonstrate significant correlation with 30-day mortality in our study. Of note, when PESI score is utilised, the majority of our study population (67%) falls into PESI Class 1 to 3, which corresponds to the group with low to moderate risk of mortality. However, when simplified PESI score is used, the majority of our study population (77%) actually falls into the high-risk category instead. This highlights our hypothesis that existing scores may have limited applicability in local and by extrapolation, Asian populations, possibly because the prevalence of cancer, heart failure and chronic lung disease in local/Asian populations are quite different from that in traditionally Caucasian study populations. In fact, the prevalence of malignancy in our study population was found to be 10% and 6.1% in another Singapore population (8) compared to 20% in overseas study populations (14).
Looking at the various markers that make up PESI and simplified PESI score, only two variables—raised respiratory rate and low oxygen saturation levels—correlated significantly with 30-day mortality in our study. The other variables—history of cancer, history of heart failure, history of chronic lung disease, tachycardia, altered mental state, hypotension and hypothermia—had no significant correlation with 30-day mortality. Nevertheless, it is important to note that although GCS score was not found have significant correlation to 30-day mortality, all patients with a GCS less than 15 did not survive beyond 30 days.
On the other hand, there were other variables not part of the PESI or simplified PESI score (e.g., raised troponin levels) which correlated significantly with 30-day mortality in our study—some of which were also found to be consistent with findings in other studies. As a marker of right ventricular dysfunction, the utility of raised troponin levels as a prognosis indicator in PE has been proven to be meaningful in both mortality and disposition outcomes (15-17). It may also be a good discriminator for outcomes in normotensive PE (18). In our study, low serum bicarbonate levels and high anion gap were significantly associated with 30-day mortality. This correlation between low bicarbonate levels and high anion gap with poorer outcomes may be attributed to the presence of lactate acidosis—one of the independent prognostic markers proposed by the SHiELD model for normotensive PE (19).
Thus, the construction of another tool to further distinguish prognosis in PE especially for the low to moderate risk groups, would be beneficial to instituting earlier treatment strategies. Our study findings may help to guide further research in developing this tool. For example, of all the various markers that make up PESI and simplified PESI score, raised respiratory rate and low oxygen saturations were the only ones found to have significant correlation to 30-day mortality, as such, they may be more meaningful to distinguish poorer outcomes. Hence, using the novel respiratory index (oxygen saturation in air to respiratory rate ratio) as part of a prognostic tool for PE severity and mortality may be prove to be more relevant (20).
In our study, early PE diagnosis is significantly associated with earlier delivery of treatment. Our overall population had earlier diagnosis (104 minutes) and therapeutics given at ED (152 minutes) compared to other published literature. Other studies reported median timing to diagnosis of 288 minutes (21) and timing to therapeutics of 756 to 978 minutes (22). Another study defined prompt timing to diagnosis as less than 2 hours (23). Forty-six (66%) patients in our study population were diagnosed within two hours.
Our study also suggests that shorter time to diagnosis and definitive therapeutics may improve mortality. While there are no statistically significant correlations, we note that the subset of our study population that survived had a shorter time to diagnosis and definitive therapeutics. This supports current research findings which suggest that initial right ventricular dysfunction may be reversible with thrombolytics (24-26). Our study encourages future prospective research to establish causative relationships and better understanding of contrast-related or bleeding complications possibly associated with earlier CT imaging and therapeutics. These serve to improve guidelines and standardize recommended timeframe to deliver therapeutics which currently varies from 11 to 411 minutes (27).
There are several limitations to our study. In view of the small study population and retrospective nature of our study, a causative relationship between the treatment factors and outcome could not be definitively determined. Being a retrospective study, our results are also limited by recall bias and accuracy of available records. In addition, the exclusion of patients with cardiopulmonary arrest may have resulted in under-representation of high-risk PE in our study population. This study ultimately serves best as a preliminary analysis to support direction of future prospective research with larger populations.
Conclusions
The study identified several factors that are significantly associated with 30-day mortality in patients presenting with acute PE to the ED. These factors are somewhat consistent with prognostic factors present in validated tools. Further research into various distinctive features of acute PE in the low to moderate risk population is required to improve future management strategies for these patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jeccm-20-96
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jeccm-20-96
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-96). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics review committee (CIRB 2018/2260) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- ISTH Steering Committee for World Thrombosis Day. Thrombosis: a major contributor to the global disease burden. J Thromb Haemost 2014;12:1580-90. [Crossref] [PubMed]
- Alotaibi GS, Wu C, Senthilselvan A, et al. Secular Trends in Incidence and Mortality of Acute Venous Thromboembolism: The AB-VTE Population-Based Study. Am J Med 2016;129:879.e19-25. [Crossref] [PubMed]
- Beydilli İ, Yilmaz F, Sonmez BM, et al. Thrombolytic therapy delay is independent predictor of mortality in acute pulmonary embolism at emergency service. Kaohsiung J Med Sci 2016;32:572-8. [Crossref] [PubMed]
- Harringa JB, Bracken RL, Nagle SK, et al. Negative D-dimer testing excludes pulmonary embolism in non-high risk patients in the emergency department. Emerg Radiol 2017;24:273-80. [Crossref] [PubMed]
- Tang Y, Sampson B, Pack S, et al. Ethnic differences in out-of-hospital fatal pulmonary embolism. Circulation 2011;123:2219-25. [Crossref] [PubMed]
- Keenan CR, White RH. The effects of race/ethnicity and sex on the risk of venous thromboembolism. Curr Opin Pulm Med 2007;13:377-83. [Crossref] [PubMed]
- Molina JA, Jiang ZG, Heng BH, et al. Venous thromboembolism at the National Healthcare Group, Singapore. Ann Acad Med Singapore 2009;38:470-8. [PubMed]
- Mok KH, Wong SW, Wong YM, et al. Clinical characteristics, risk factors and outcomes of South-East Asian patients with acute pulmonary embolism. Int J Cardiol 2017;249:431-3. [Crossref] [PubMed]
- Jen WY, Jeon YS, Kojodjojo P, et al. A New Model for Risk Stratification of Patients With Acute Pulmonary Embolism. Clin Appl Thromb Hemost 2018;24:277S-84S. [Crossref] [PubMed]
- Zhou XY, Ben SQ, Chen HL, et al. The prognostic value of pulmonary embolism severity index in acute pulmonary embolism: a meta-analysis. Respir Res 2012;13:111. [Crossref] [PubMed]
- Aujesky D, Obrosky DS, Stone RA, et al. Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med 2005;172:1041-6. [Crossref] [PubMed]
- Donzé J, Le Gal G, Fine MJ, et al. Prospective validation of the Pulmonary Embolism Severity Index. A clinical prognostic model for pulmonary embolism. Thromb Haemost 2008;100:943-8. [Crossref] [PubMed]
- Jiménez D, Aujesky D, Moores L, et al. Simplification of the pulmonary embolism severity index for prognostication in patients with acute symptomatic pulmonary embolism. Arch Intern Med 2010;170:1383-9. [Crossref] [PubMed]
- Heit JA, O'Fallon WM, Petterson TM, et al. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch Intern Med 2002;162:1245-8. [Crossref] [PubMed]
- Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Respir J 2019;54:1901647. [Crossref] [PubMed]
- Amorim S, Dias P, Rodrigues RA, et al. Troponin I as a marker of right ventricular dysfunction and severity of pulmonary embolism. Rev Port Cardiol 2006;25:181-6. [PubMed]
- Margato R, Carvalho S, Ribeiro H, et al. Cardiac troponin I levels in acute pulmonary embolism. Rev Port Cardiol 2009;28:1213-22. [PubMed]
- Zhu L, Wang C, Yang YH, et al. Prognostic value of right ventricular dysfunction and derivation of a prognostic model for patients with acute pulmonary thromboembolism. Zhonghua Liu Xing Bing Xue Za Zhi 2009;30:184-8. [PubMed]
- Freitas P, Santos AR, Ferreira AM, et al. Derivation and external validation of the SHIeLD score for predicting outcome in normotensive pulmonary embolism. Int J Cardiol 2019;281:119-24. [Crossref] [PubMed]
- Vedovati MC, Cimini LA, Pierpaoli L, et al. Prognostic value of respiratory index in haemodynamically stable patients with acute pulmonary embolism: The Respiratory Index model study. Eur Heart J Acute Cardiovasc Care 2020;9:286-92. [Crossref] [PubMed]
- Smith SB, Geske JB, Morgenthaler TI. Risk factors associated with delayed diagnosis of acute pulmonary embolism. J Emerg Med 2012;42:1-6. [Crossref] [PubMed]
- Chaudhury P, Gadre SK, Schneider E, et al. Impact of Multidisciplinary Pulmonary Embolism Response Team Availability on Management and Outcomes. Am J Cardiol 2019;124:1465-9. [Crossref] [PubMed]
- Bach AG, Bandzauner R, Nansalmaa B, et al. Timing of pulmonary embolism diagnosis in the emergency department. Thromb Res 2016;137:53-7. [Crossref] [PubMed]
- Smith SB, Geske JB, Maguire JM, et al. Early anticoagulation is associated with reduced mortality for acute pulmonary embolism. Chest 2010;137:1382-90. [Crossref] [PubMed]
- Kline JA, Hernandez-Nino J, Jones AE, et al. Prospective study of the clinical features and outcomes of emergency department patients with delayed diagnosis of pulmonary embolism. Acad Emerg Med 2007;14:592-8. [Crossref] [PubMed]
- Kausar S, Khan HS, Nazir MTB, et al. Acute Pulmonary Embolism: Presentation, Diagnosis, Management and Factors Impacting Clinical Outcome in a Tertiary Cardiac Centre in Pakistan. J Coll Physicians Surg Pak 2019;29:749-52. [Crossref] [PubMed]
- Pollack CV, Schreiber D, Goldhaber SZ, et al. Clinical characteristics, management, and outcomes of patients diagnosed with acute pulmonary embolism in the emergency department: initial report of EMPEROR (Multicenter Emergency Medicine Pulmonary Embolism in the Real World Registry). J Am Coll Cardiol 2011;57:700-6. [Crossref] [PubMed]
Cite this article as: Soo JEJ, Takashima K, Tiah L, Leong BYG. Factors associated with mortality among Asian patients diagnosed with acute pulmonary embolism in the Emergency Department. J Emerg Crit Care Med 2021;5:4.



