Role of fluoroscopy re-emphasized in guiding dual lumen extracorporeal membrane oxygenation catheter insertion
The advantages of a dual-lumen jugular vein extracorporeal membrane oxygenation (ECMO) catheter include single vessel placement, minimal recirculation and the potential for early patient mobilization (1). Despite all these advantages, its application remains limited by the large cannula size and more importantly, the sophisticated imaging techniques required to ensure safe cannulation and to guide optimal catheter depth and positioning. In our center, dual-lumen ECMO catheter cannulation is reserved for those running out of vascular accesses.
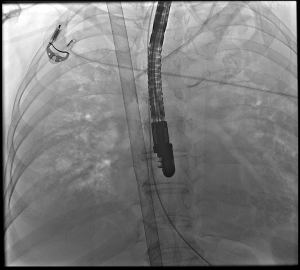
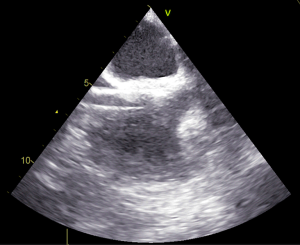
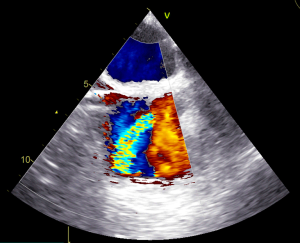
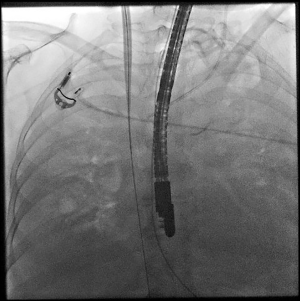
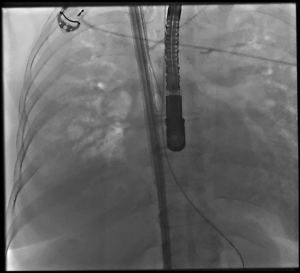
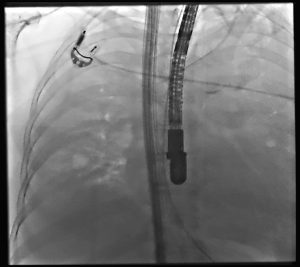
More and more articles have been reporting on the successful insertion of dual-lumen ECMO catheter under transesophageal echocardiography (TEE) guidance alone. From the practical point of view, most patients requiring veno-venous ECMO initiation are too ill for transport to the fluoroscopy suit, and meanwhile fluoroscopy service is not as readily available as TEE in intensive care units. Hemamalini el al. reported their experience of dual lumen catheter insertion in 10 patients, with half using TEE guidance and half using fluoroscopy guidance (2). Despite their conclusion that TEE being the ideal imaging modality for guidance, the image guiding and the catheter insertion techniques themselves were highly operator dependent and the results from the study design were far from conclusive. Some of the reported complications in their fluoroscopy guidance group could be potentially avoidable too. They reported 4 out of 5 patients with low flow at initiation of ECMO, with 2 catheters lodged in the heparin veins, 1 catheter lodged in the inferior vena-cava junction and one catheter kinked. Our group believe that these complications should be more easily visualize under fluoroscopy, as compared with TEE, which provides limited field of view. Moreover, there have been various case reports reporting different cardiac complications from misplacement of the dual-lumen ECMO catheters during cannulation, resulting in lethal catastrophe (3,4). For a lot of these cases, the insertions were already well guided by TEE. Our group would like to share a few limitations of this TEE guided technique. Firstly, the depth of the guidewire insertion in the inferior vena cava (IVC) beyond the right atrium (RA) cannot be well assessed. Usually only few centimeters of the IVC below the RA can be visualized in the bi-caval view. Sufficient length of guidewire should be allowed in the IVC so that the chance of it inadvertently jumping to the RA, or even to the right ventricle, is minimized. Moreover, the complete visualization of the guidewire course prevents it from being lodged accidentally in the heparin vein or other areas as described (2). This is especially the case during guidewire manipulation, dilatation, and catheter insertion, when the drifting movement of the guidewire can cause vascular injuries. Secondly, the soft J-tipped guidewires provided in most commercially available dual-lumen ECMO catheter sets, which are designed for possible bedside percutaneous cannulation, do not have adequate stiffness to allow easy insertion of large-bore catheters by Seldinger’s technique. This is especially the case when the dual-lumen catheters are usually of sizes larger than 30 Fr. Teman et al. have also reported the possibility of guidewire looping in the right heart chambers during guidewire manipulation (5). Meanwhile, kinking of the guidewires during dilatation of soft tissue tracks can result in false tracking. With TEE guidance alone, insertion of stiff guidewire without full visualization of the course can result in vascular injuries (3). Thirdly, visualization of the return port of the ECMO catheter in TEE is more easily said than done. Figure 1 shows the image at the level of the return port and the readers can appreciate how difficult it is to confirm its position (Figure 1). It is just shown as a few centimeters of radiolucency. 3D Echocardiography might help in this area, but such technique might not be readily available in each ECMO center. Some proposed the use of agitated saline test by flushing the return lumens (6), while Doppler assessment done after the ECMO circuit is established can assist fine adjustment of the positioning (Figure 2), but they required extra catheter manipulations in a patient who is already highly unstable. We in this article would like to re-emphasize the importance of fluoroscopic guidance during dual-lumen ECMO catheter insertion, especially focusing on guiding the safe use of stiff guidewire assisted Seldinger’s technique and the proper guidance to the catheter insertion depth and positioning. After puncturing at the right internal jugular vein, a soft tipped J wire is inserted under fluoroscopy guidance. The guidewire is passed below the diaphragm and should be deep enough below the heart silhouette to allow length for guidewire manipulation (Figure 3). To exchange for a stiff guidewire to get extra support in the Seldinger’s technique, a 5-Fr Judkins Right (JR4) coronary diagnostic catheter, (Figure 4) which is readily available in every cardiac catheterization laboratory used for performing diagnostic coronary angiography, can be inserted as a conduit to exchange for a stiff guidewire. This catheter exchange technique avoids potential vascular injury inherited during stiff guidewire insertion. During insertion of dilatators or the catheter, traction on the stiff guidewire by another operator should be maintained and the movement of the guidewire should be kept minimal. The direction as of the dilator or catheter insertion should be guided by direct visualization of the course of the guidewire under fluoroscopy (Figure 5). The deep position of the guidewire in the IVC and the stiffness of the guidewire well prevent the guidewire from inadvertent jumping to the RA. The next consideration is how to visualize the return side-port of the ECMO catheter under fluoroscopy and thus guide the depth and positioning of the catheter. Figure 6 shows the Cine film the catheter. A cine film provides better image quality compared with usual fluoroscopy at the expense of more radiation. Despite that, it is still difficult to locate the return port on the catheter (Figure 6). One of the main reasons is that if the port is not at right angle to the imaging plane, the radiolucency of the return port is difficult to recognize. Without knowledge of the position of the return port, it is difficult for the operator to determine the depth of catheter insertion. One possible solution is using X-ray contrast. However, a large volume of contrast and long fluoroscopy time is needed due to the large catheter dead space. Multiple injection might also be needed during fine position adjustment. A simple method we employ is to insert a guidewire through the return lumen of the catheter, and the guidewire will mark the return port at the position it loses track with the ECMO catheter (Figure 7). The catheter is then inserted with the return lumen sitting at the RA, facing the tricuspid valve (Figure 8). With this, the positioning of the catheter is usually near optimal. Further fine tuning can be done with Doppler assessment after the circuit is running, and usually transthoracic echocardiography assessment suffices.

Conclusions
It is possible to perform safe and accurately positioned dual-lumen ECMO catheter insertion using fluoroscopic guidance alone. Fluoroscopy can also supplement TEE guidance by giving additional information. Our group would highly recommend its use as far as possible.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-184). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees, and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient’s relatives.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang D, Zhou X, Liu X, et al. Wang-Zwische double lumen cannula-toward a percutaneous and ambulatory paracorporeal artificial lung. ASAIO J 2008;54:606-11. [Crossref] [PubMed]
- Hemamalini P, Dutta P, Attawar S. Transesophageal Echocardiography Compared to Fluoroscopy for Avalon Bicaval Dual-Lumen Cannula Positioning for Venovenous ECMO. Ann Card Anaesth 2020;23:283-7. [Crossref] [PubMed]
- Banayan JM, Barry A, Chaney MA. Right Ventricular Rupture during Insertion of an Avalon Elite(®) Catheter. J Cardiothorac Vasc Anesth 2016;30:e34-e35. [Crossref] [PubMed]
- Hirose H, Yamane K, Marhefka G, et al. Right ventricular rupture and tamponade caused by malposition of the Avalon cannula for venovenous extracorporeal membrane oxygenation. J Cardiothorac Surg 2012;7:36. [Crossref] [PubMed]
- Teman NR, Haft JW, Napolitano LM. Optimal endovascular methods for placement of bicaval dual-lumen cannulae for venovenous extracorporeal membrane oxygenation. ASAIO J 2013;59:442-7. [Crossref] [PubMed]
- Hayes D Jr, Preston TJ, Davis IC, et al. Contrast transthoracic echocardiography and the placement of a bicaval dual-lumen catheter in a Swine model of venovenous extracorporeal membrane oxygenation. Artif Organs 2013;37:574-6. [Crossref] [PubMed]
Cite this article as: Au SY, Fong KM, Tsui THJ, Sin KC, Ng WG, Leung KA. Role of fluoroscopy re-emphasized in guiding dual lumen extracorporeal membrane oxygenation catheter insertion. J Emerg Crit Care Med 2021;5:16.