
Use of high flow oxygen (HFO) for difficult airway management in Jael syndrome: a case report
Introduction
Jael syndrome is named for a woman from the Bible. According to the verse, Jael killed Sisera, Commander of the Canaanite army, by driving a tent peg using a hammer into his temple (1).
There are only a few cases in the medical literature describing face impalement with the presence of the instrument in the face. Jael syndrome was first reported by Jefferson in 1968 when reporting the case of a 16 years old impaled with a tent peg (2), and was later defined by Harris et al., in 1988, as an intentional craniofacial stab injury (3).
Jael syndrome is a rare occurrence. Very few trauma centres would have adequate experience in the management of such injuries. The management is multidisciplinary involving pre-hospital health care professionals, maxillofacial surgeons, radiologists, anaesthetists, intensive care physicians and, in some instances, neurosurgeons.
The management of these cases can be particularly challenging as the patients are often anxious, under the influence of alcohol or illicit drugs. Depending on the extent and depth of penetration, the instrument may be either removed under local anaesthesia or general anaesthesia (4,5). In deep penetrating injuries necessitating a general anaesthetic, one of the most challenging aspects is safe airway management (6-8).
The use of HFO in anaesthesia is a relatively recent development. Here, we discuss a case describing the first documented use of high flow oxygen in pre-oxygenating and the intubation of a patient with Jael Syndrome. We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jeccm-20-47).
Case presentation
A 20 years old male walked into the emergency department after being stabbed with a large kitchen knife in his left maxilla with the knife blade still in situ. He was a smoker and recreational consumer of alcohol, however he had no other past medical history nor was on any long term medications.
On arrival he was fully conscious, haemodynamically stable with no apparent airway compromise.
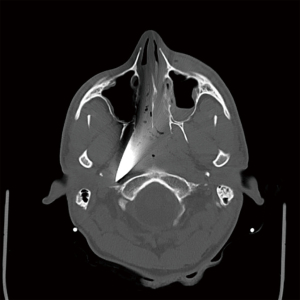
He underwent a CT head scan which showed that 12.5 cm of the knife was buried transfacially, penetrating through the left maxilla below the infraorbital margin and orbital floor (Figure 1). It traversed the left lateral nasal wall and nasal septum, crossing the contralateral nasopharynx and was embedded into the right occipital condyle at the base of skull. The point of the knife lay medial to the carotid sheath which contains the internal carotid artery, internal jugular vein and cranial nerves IX-XII (Figure 2). He did not reveal any “hard signs” that are described for immediate transfer to the operating room. He had a secondary survey completed and cross matched 4 units.
He was then transferred to the operating room to remove the knife and arrest any bleeding. At induction, preoperative antibiotics and tranexamic acid were administered intravenously.
With such a large foreign body protruding from his maxilla, it seemed to be difficult to pre-oxygenate or to bag-mask-valve ventilate the patient with a tight fitting mask. Our proposed plans for intubation were awake fibre-optic intubation, awake tracheostomy or RSI using video laryngoscopy and pre-oxygenation of with HFO administered via a Hudson mask. The blockage of the nostrils with blood and the blade precluded the use of nasal cannula.
He was pre-oxygenated for five minutes using HFO through a Hudson mask at a flow rate of 60 L/min (Figure 3).Following pre-oxygenation, the patient underwent rapid sequence induction using Fentanyl 100 mcg/Propofol 200 Mg/Rocuronium 90 mg Sugummadex and a Laryngeal Mask Airway were available to be used in case of failed intubation. HFO delivery was maintained throughout induction until satisfactory intubation conditions were achieved.
He was intubated using a glidescope whilst maintaining manual in-line stabilisation of his cervical spine. Due to the presence of the protruding knife, the intubation was technically difficult and was successful after the third attempt using the glidescope. Total apnoea time was three minutes. Throughout the period of apnoea his oxygen saturations remained at 99%. After intubation the first end tidal carbon dioxide concentration obtained was 5.4 kPa. No immediate adverse effects were observed.
He then underwent the surgical removal of the blade. The blade length was measured to be 20 cm with 12.5 cm impaling the patient’s faces. Haemorrhage was controlled by local measures and the nasopharynx was initially packed with anterior and posterior RapidRhino® packs. They were replaced using two 18Fr Foley urinary catheters both inflated to 30ml, to tamponade the tissues on the lateral and posterior aspect of the nasopharynx. An anterior RapidRhino® was packed in the left nostril. Packing was kept in situ for 48 hours. At the time of the surgery, measurements of the knife of the length and penetration were recorded as part of the detailed medicolegal report. The offending article was placed into a sealed forensics bag for further forensic analysis. The following day the patient underwent a CT angiogram which showed a small air bubble in the right carotid space at the site of the tip of the removed blade, with no active extravasation nor signs of pseudoaneurysms. It was noted that there was a haematoma in the left cheek region and a left maxillary haemosinus. In addition, the CT showed mildly displaced fractures in the anterior and medial walls of the left maxillary sinus.
He was sedated and ventilated in the intensive care unit for a total of 33 hours. Subsequently he was extubated and later transferred to the ward for further management.
He was discharged from hospital 2 days later, and subsequently reviewed in maxillofacial outpatient clinic. He was assessed for cranial nerve deficit and only exhibited anaesthesia on the left infraorbital nerve distribution, and reported a feeling of occasional loss of balance but no vertigo. This had resolved on third follow-up appointment one month post discharge. He had suffered no adverse effects secondary to treatment.
A timeline of his care is summarised in Table 1. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution and national research committees, and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
Table 1
| Date | Time | Patient event |
|---|---|---|
| 12/04/2019 | 2234 hrs | Patient presented to Emergency Department following stabbing with large knife protruding from left maxilla |
| 12/04/2019 | 2303 hrs | Initial diagnostic CT scan shows knife penetrating left maxilla, extending 12.5 cm traversing across the nasal septum and contralateral nasopharynx, and embedded in the right occipital condyle |
| 12/04/2019 | 2350 hrs | Admission to operating theatre |
| 13/04/2019 | 0002 hrs | Preoxygenation with HFO |
| 13/04/2019 | 0010 hrs | Induction of anaesthesia and intubation after 3rd pass using glidescope. Oxygen saturations maintained at 99% throughout period of apnoea |
| 13/04/2019 | 0013 hrs | First ETCO2 recording of 5.4 |
| 13/04/2019 | 0025 hrs | Operation start time-knife removed, haemorrhage control achieved with packing nasopharynx with anterior and posterior RapidRhino® packs and then bilateral Foley catheters. |
| 13/04/2019 | 0133 hrs | Discharge from operating theatre |
| 13/04/2019 | 0134 hrs | Admitted to ITU, remained intubated and ventilated |
| 13/04/2019 | 1202 hrs | Follow up CT Angiogram shows small air bubble at right carotid space, anteromedial to right internal carotid artery, but no active extravasation or signs of pseudo-aneurysms; mildly displaced fractures of left maxillary sinus anterior and medial walls noted |
| 14/04/2019 | 1108 hrs | Extubation on ITU |
| 14/04/2020 | 1444 hrs | Discharge from ITU |
| 16/04/2020 | Discharge from hospital after maxillofacial review | |
| 17/04/2020 | First review in maxillofacial outpatients, reports numbness over left upper anterior teeth | |
| 02/05/2019 | Second review in maxillofacial outpatients, reports occasional sensation of loss of balance with no vertigo symptoms; formal examination normal | |
| 30/05/2020 | Third review and discharge from maxillofacial outpatients, balance issues resolved, ongoing sensory issues in left infra-orbital nerve distribution |
Discussion
HFNO/HFO is a relatively novel technique for oxygen therapy providing more beneficial results compared to conventional oxygen therapy devices. The system is composed of an oxygen/air blender connected via an active heated humidifier to a nasal cannula, through a single-limb heated inspiratory circuit. It delivers a fraction of inspired oxygen (FiO2) from 21% to 100%, with a flow rate up to 60 L/min (9).
Although the mechanism of action of HFO is not fully understood it maintains oxygenation by providing high flows of gas. The high flow also creates positive airway pressure correlating with the flow rate (10-13). This high airway pressure improves oxygenation throughout the respiratory cycle, an effect than can be compared to the application of PEEP. It also acts to produce a reduction of dead space ventilation by the washout of the nasopharyngeal dead space volume (14,15). Due to the humidification and warming of the delivered oxygen, HFO is well tolerated and leads to improved mucociliary function and secretion clearance compared to conventional oxygen therapy devices (16,17).
The use of HFO has extended beyond its original scope in neonatal and paediatric patients to encompass both ITU and theatre settings. Evidence has shown it to be safe in the delivery of pre-oxygenation prior to RSI (18,19). Patel et al. were able to show that its use can increase the safe apnoea time in patients with a predicted difficult airway, proposing that it reduces the chance of desaturation by apnoeic oxygenation with gaseous exchange via dead space flushing (20). Its use in this case of maxillofacial trauma allowed for the adequate preoxygenation and apnoeic oxygenation and therefore a prolonged intubation window in what would otherwise be technically difficult circumstances.
Whilst the use of HFO has been shown to be efficacious in RSI and induction of anaesthesia, there are limitations in its use, particularly in the trauma patient. The nature of the injuries in our case necessitated the delivery of oxygen via a specialised mask, as the more commonly used nasal route was compromised. The use of HFO is also contraindicated in cases where the patient is suspected to have suffered from a base of skull fracture or open communication to the intracranial space. Likewise, consideration needs to be given to the presence of epithelial/mucosal injuries of the airway and presence of pneumothoraces.
Conclusions
The use of high flow oxygen should be considered as part of the management plan in providing pre-oxygenation and increased safe apnoea time in patients with penetrating maxillofacial injuries requiring intubation.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jeccm-20-47
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-47). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- The King James Bible, Book of Judges Chapter 4: Verse 21.
- McKechnie J. A severe craniofacial impalement injury (Jael's syndrome). Br J Oral Maxillofac Surg 1986;24:258-64. [Crossref] [PubMed]
- Harris A M P, Wood RE, Nortje CJ, et al. Deliberately inflicted penetrating Injuries of the maxillofacial region (Jael's syndrome). J Craniomaxillofac Surg 1988;16:60-3. [Crossref] [PubMed]
- Voss JO, Thieme N, Doll C, et al. Penetrating Foreign Bodies in Head and Neck Trauma: A Surgical Challenge. Craniomaxillofac Trauma Reconstr 2018;11:172-82. [Crossref] [PubMed]
- Santos Tde S, Melo AR, de Moraes HH, et al. Impacted foreign bodies in the maxillofacial region-diagnosis and treatment. J Craniofac Surg 2011;22:1404-8. [Crossref] [PubMed]
- Coppola S, Froio S, Merli G, et al. Maxillofacial trauma in the emergency department: pearls and pitfalls in airway management. Minerva Anestesiol 2015;81:1346-58. [PubMed]
- Barak M, Bahouth H, Leiser Y, et al. Airway Management of the Patient with Maxillofacial Trauma: Review of the Literature and Suggested Clinical Approach. Biomed Res Int 2015;2015:724032 [Crossref] [PubMed]
- Jain U, McCunn M, Smith CE, et al. Management of the Traumatized Airway. Anesthesiology 2016;124:199-206. [Crossref] [PubMed]
- Ischaki E, Pantazopoulos I, Zakynthinos S. Nasal high flow therapy: a novel treatment rather than a more expensive oxygen device. Eur Respir Rev 2017;26:170028 [Crossref] [PubMed]
- Ritchie JE, Williams AB, Gerard C, et al. Evaluation of a humidified nasal high-flow oxygen system, using oxygraphy, capnography and measurement of upper airway pressures. Anaesth Intensive Care 2011;39:1103-10. [Crossref] [PubMed]
- Parke R, McGuinness S, Eccleston M. Nasal high-flow therapy delivers low level positive airway pressure. Br J Anaesth 2009;103:886-90. [Crossref] [PubMed]
- Groves N, Tobin A. High flow nasal oxygen generates positive airway pressure in adult volunteers. Aust Crit Care 2007;20:126-31. [Crossref] [PubMed]
- Parke RL, Eccleston ML, McGuinness SP. The effects of flow on airway pressure during nasal high-flow oxygen therapy. Respir Care 2011;56:1151-5. [Crossref] [PubMed]
- Möller W, Celik G, Feng S, et al. Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol 2015;118:1525-32. [Crossref] [PubMed]
- Möller W, Feng S, Domanski U, et al. Nasal high flow reduces dead space. J Appl Physiol 2017;122:191-7. [Crossref] [PubMed]
- Williams R, Rankin N, Smith T, et al. Relationship between the humidity and temperature of inspired gas and the function of the airway mucosa. Crit Care Med 1996;24:1920-9. [Crossref] [PubMed]
- Hasani A, Chapman TH, McCool D, et al. Domiciliary humidification improves lung mucociliary clearance in patients with bronchiectasis. Chron Respir Dis 2008;5:81-6. [Crossref] [PubMed]
- Mir F, Patel A, Iqbal R, et al. A randomised controlled trial comparing transnasal humidified rapid insufflation ventilatory exchange (THRIVE) pre-oxygenation with facemask pre-oxygenation in patients undergoing rapid sequence induction of anaesthesia. Anaesthesia 2017;72:439-43. [Crossref] [PubMed]
- Raineri SM, Cortegiani A, Accurso G, et al. Efficacy and Safety of Using High-Flow Nasal Oxygenation in Patients Undergoing Rapid Sequence Intubation. Turk J Anaesthesiol Reanim 2017;45:335-9. [Crossref] [PubMed]
- Patel A, Nouraei SA. Transnasal. Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia 2015;70:323-9. [Crossref] [PubMed]
Cite this article as: Browne C, Mujitaba A, Pilkington R, Putnam G, Barberis L. Use of high flow oxygen (HFO) for difficult airway management in Jael syndrome: a case report. J Emerg Crit Care Med 2021;5:35.




