
Forty-eight-hour hospital mortality: an emergency department perspective studying the relationship between suboptimal care and mortality
Introduction
There has been increasing emphasis in the recent decades to improve patient safety in hospitals and to minimise adverse events. The aim of this is to avoid preventable deaths for patients admitted to hospital (1) whether as an emergency or an elective admission.
Many studies in the USA have looked at the rates of patient deaths resulting from the medical care that patients received. In 1999 the Institute of Medicine in the United States reported a potential 98,000 deaths per year due to medical errors (2). Landrigan et al. estimated that 0.7% of hospital admissions over a six-year period in North Carolina in USA resulted in lethal adverse events (3).
In the UK in 2000 the Chief Medical Officer published a report which estimated that 60,000 to 255,000 NHS patients were seriously disabled or died every year as a result of healthcare interventions (4). A study by Hogan et al. of 1,000 patients reported that 5.2% of deaths were potentially preventable. If these results were extrapolated for all acute trusts across England this could be in excess of 11,000 preventable deaths (5).
Following publication of the Care Quality Commission’s report on Patient Safety in 2016, the UK Health Secretary made it compulsory for all NHS Trusts and Foundation Trusts in England to collect information on serious incidents and deaths that were potentially avoidable to consider lessons that could be learnt (6).
Most deaths that occur in hospitals can be predictable due to the underlying presenting pathology of the patient. However some deaths can be avoided by improving the care that patients receive (7).
Hospital mortality, with death as an endpoint is one of the statistics used throughout the health service to ascertain the quality of care being delivered to patients.
The widely used Hospital Standardised Mortality Ratios (HSMR) in Scotland or the Summary Hospital Mortality Indicators (SHMI) in England looks at the ratio of observed deaths to expected deaths within 30 days of hospital admission taking into account factors known to affect the underlying risk of death (7-9). However it should not be used in isolation to evaluate the care provided to this group of patients, due to the risk of false positives or negatives.
In order to determine the prevalence of patient mortality secondary to the provision of suboptimal care this study was undertaken. The main objective was to ascertain if the care that the patients received in the Emergency Department (ED) or soon after hospital admission resulted in an adverse outcome. As a result, all inpatient deaths that occurred within 48 hours of hospital admission were studied. It was anticipated that a 48-hour time period would be reflective of the initial care that the patient had received in the ED.
Following recognition of an adverse outcome, mechanisms were instituted to prevent or minimise such occurrences in future.
The secondary objective of the study was to ascertain if there was any relationship between adverse outcome and the day of admission, time of admission and time to first assessment (TTFA).
To our knowledge this is the first study in the UK and worldwide in assessing death within 48 hours of hospital admission with the aim of using this as a learning tool and implementing strategies to prevent similar incidents in future.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jeccm-20-172).
Methods
This retrospective cohort study was carried out in a single acute hospital site in National Health Service Lanarkshire (NHSL) from the 1st of January 2015 to the 31st of December 2018.
Inclusion criteria was patients over the age of 16 years presenting via the ED and subsequently dying within 48 hours of hospital admission. Hospital admission is defined as when the patient leaves the ED following initial management and treatment and is transferred into a ward bed, theatre or an interventional radiology or cardiology suite. Patients referred directly to supporting specialities by the General Practitioner (GP) and direct referrals to the Primary Percutaneous Cardiology Intervention (PPCI) from regional hospitals or the Scottish Ambulance Service (SAS) were excluded from the study. Weekend admission was classified as 00:00 h Saturday to 23:59 h Sunday, and out of hours (OOH) as 00:00 to 07:59 h daily.
A retrospective case record review (RCCR) was done within 3 months of the patient’s death to allow discussion and determination of potential external influences that may have contributed to the patient’s death. The patient’s electronic medical and nursing records in addition to laboratory and radiological results for the current hospital admission were reviewed.
In order to reduce inter-observer variability a single assessor—a senior ED consultant—undertook the RCCR for all patients. The assessor after a RCCR determined a death classification category for the patient as per the NHSL Mortality Review Form (10). Death was classified into one of four categories based on whether death was a likely or unlikely outcome and whether appropriate management had or had not been undertaken. Deaths attributed to classification 1 and 3 for the purposes of the study were termed ‘optimal care provided’ and deaths attributed to classifications 2 and 4 were termed ‘suboptimal care provided’. Therefore, if a death was deemed to be due to suboptimal care (classification 2 or 4), a further review was mandated (Table 1).
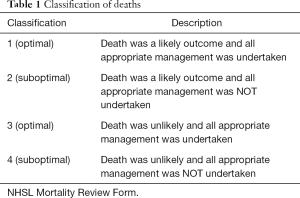
Full table
Statistical analysis
SPSS version 23 was used for statistical analysis. Pearson Chi squared tests were used for nominal and ordinal variables
Results
During the study period there were 83,825 emergency admissions to hospital, of whom 4,251 (0.05%) died within 30 days of admission (Figure 1).
Of the 4,251 emergency admissions that died within 30 days, 663 (16%) patients died within 48 h of hospital admission. Of these 663 patients, 169 (25%) were GP referrals to medical and surgical specialities. These patients were admitted via the ED to hospital for ongoing care by the receiving speciality; 57 (9%) patients were direct referrals to the PPCI suite. These patients did not come via the ED.
A total of 437 (66%) patients were eligible for the study as they had been initially assessed and managed by the ED team. Case notes were missing for 2 patients and were therefore excluded from further analysis.
Patient demographics and cause of death
Of the 435 patients studied, 232 were male and 203 were female. The ages ranged from 16 to 103 years with a median age of 75 years; 401 (92%) of deaths were deemed to have had optimal care whereas 34 (8%) patients had provision of suboptimal care (Table 2); 26 (74%) of the 34 patients in the suboptimal care group could have had their care improved in the ED. There was no statistical significant association between sex of individuals and quality of care received (P=0.166). Patients who had provision of optimal care had a median age of 76 years compared to 69 years in patients in whom suboptimal care was provided. There was no statistically significant association between age of patients and quality of care received (P=0.488) (Table 2).
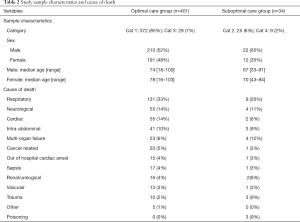
Full table
Deaths were most commonly due to the respiratory, neurological, cardiac or intra-abdominal systems in both groups. However deaths attributed to multi-organ failure (MOF), trauma and poisoning appeared more common in the suboptimal care group compared to the optimal care group. The numbers were too small in some groups to allow statistical analysis (Table 2).
Effect of day of admission, time of ED presentation and TTFA
Day of ED admission
There was no statistical significance (P=0.68) that weekend presentation to the ED resulted in a higher number of patients in the suboptimal care group compared to optimal care group (Table 3).
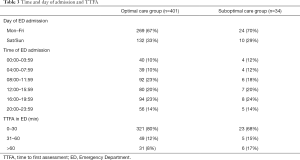
Full table
Time of ED presentation
Time of initial ED presentation was analysed in 6×4 hourly blocks. In both groups of patients there were more admissions during daytime compared to late evening and OOH. There were no statistical differences between the two groups (P=0.97) (Table 3).
TTFA in ED
The majority of patients were assessed within 30 minutes of arrival with 80% in optimal care group compared to 67% in suboptimal care group. The number of patients for both groups reviewed after one hour diminished markedly. There was no association between TTFA in ED and level of care received (P=0.97) (Table 3).
Action undertaken
Once a patient was allocated to the suboptimal care group further multi-disciplinary evaluation was then undertaken at the next ED Mortality and Morbidity Review Meeting. This resulted in additional action then being commenced either at an individual, departmental, speciality, or at a hospital wide based level. Issues with the pre-hospital care were also discussed at the appropriate pre-hospital forums. Examples of the some of the actions (but not limited to) that took place are as listed (Table 4) with some patients requiring more than one action.
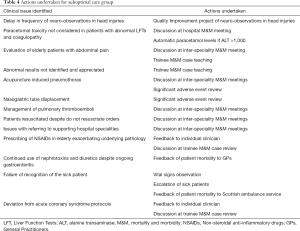
Full table
Discussion
Currently mortality in NHS Scotland is measured using HSMR. HSMR is a useful indicator for a hospital to measure its mortality trend over a given period of time (7,8). However it provides no information about the quality of care provided to individual patients.
Another method of looking at deaths is by a RCCR. This is done through an analysis of the contents of the care record of the patient and can give a more meaningful indication of the quality of the care that patients receive (11). These can be more valuable in changing hospital and departmental systems and to enhance learning to prevent errors occurring in future - thus improving patient care.
Our study is the first study to date looking at deaths of patients who present acutely to an ED and subsequently die within 48 h of hospital admission. In our opinion the 48-hour time frame is a useful proxy marker of the urgent and immediate care delivered to patients in an ED. A RCCR done within 3 months of the patient’s death allowed a timely review to ascertain if the care delivered in the ED or soon after hospital admission could have been improved.
We found that 34 (8%) of the 435 patients received suboptimal care. Action was undertaken in 33 (97%) of the 34 patients as a direct result of this study. Action undertaken was either/and at an individual, departmental, hospital or health board level to minimise risk in future.
Hogan et al. RCCR of 1,000 adult patient deaths in 10 acute hospitals in England concluded that 5.2% of deaths could have been preventable (5). However unlike our study, once issues were identified it is unclear what action if any was taken. Similarly Landrigan’s study concluded that despite recognition of patient safety issues there was no evidence of implementation of safety systems (3).
Whilst a RCCR study is laborious and time consuming it does provide an analysis of where the failings in patient care have occurred. It is only once the failings have been identified that patient safety systems can be robustly improved. This requires input from all clinical and managerial levels of the hospital and pre-hospital structures.
A study by Freemantle looked at the 30-day mortality of elective and emergency admissions and concluded that there was an increased risk of death of admission at the weekend (12). This study was often deemed to be widely quoted by the UK Health Secretary during implementation of a new junior doctors’ contract in 2016 (13). This aim of this contract was to improve patient outcomes across the week by extending the standardised working weekday and part of the weekend (7). However in our study there was no evidence that emergency admission at the weekend or OOH was associated with an increased mortality secondary to adverse clinical care when admitted via the ED.
A total of 348 (80%) of 435 patients presented to the ED between 08:00 h and midnight with a fairly equal distribution throughout the day followed by a slight reduction in the late evening. This is reflective of the general pattern of patient attendances to our ED.
Consideration was given to the possibility of those admissions to the ED between 00:00 and 08:00 h may be associated with an adverse patient outcome as ED consultants are not routinely present in the ED at this time. However the study found no evidence of this.
A total of 261 (60%) of the 435 patients had a pre-alert call by the SAS, highlighting the significance of early recognition of the unwell patient by the SAS personnel. This ensured that the ED resuscitation team was present to commence immediate management of the patient on arrival to the department.
In total, 344 (79%) of all our emergency admissions to the ED were seen and assessed by a medical staff member within 30 minutes of arrival. In one patient in the sub-optimal care group, the delayed TTFA was a contributory factor to the patient’s demise.
Thus our study has revealed that after an in depth RCCR over a 4 year period, 6% of patients could have had their care improved and in 2% of patients death was potentially avoidable. Importantly action has been taken to mitigate these in future.
Limitations
The limitations of the study were that there was one person only doing the initial case record review, there was exclusion of elective and speciality patients in addition to patients directed to other clinical areas and finally the study did not look at medical staffing ratios and whether that may have impacted on the results.
Conclusions
Clear evidence has been found for doing a robust RCCR for inpatient hospital deaths as a means to implementing change to improving patient care and minimising future patient risk. A shortened time period of 48 hours after emergency hospital admission allowed the study centre to identify and undertake appropriate action to minimise such incidences in the future.
We would recommend that all acute hospitals undertake an ongoing evaluation similar to this one—in conjunction with HSMR or SHMIs—with the primary aim of implementing improvements if suboptimal care is identified. It is advocated that specific time and support is given to senior medical staff to allow this to happen across all specialities, with findings shared to enhance patient care throughout the healthcare setting.
Finally in the current global pandemic situation due to Covid-19, it will be more important than ever to ensure that high quality care continues to be delivered to all groups of patients.
Acknowledgments
I would like to thank all ED consultants (in particular Dr. Julie Cash) who supported the study and helped in the implementation of changes. Thank you also to the supporting specialities within the hospital.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jeccm-20-172
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jeccm-20-172
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-172). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was a review of the clinical service delivered, with the ultimate aim of improving quality of care. It was not considered to be research by the NHS Health Research Authority decision guide tool and therefore ethical approval was not sought. As this was a retrospective review of 48-hour mortality after emergency hospital admission patient this research was done without patient involvement.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kavanagh KT, Saman DM, Bartel R, et al. Estimating Hospital-Related Deaths Due to Medical Error: A Perspective From Patient Advocates. J Patient Saf 2017;13:1-5. [Crossref] [PubMed]
- Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Washington, DC: National Academic Press, 1999.
- Landrigan CP, Parry GJ, Bones CB, et al. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med 2010;363:2124-34. [Crossref] [PubMed]
- National Institute for Health and Care Excellence. Eyes on Evidence. January 2013.
- Hogan H, Healey F, Neale G, et al. Preventable deaths due to problems in care in English acute hospitals: a retrospective case record review study. BMJ Qual Saf 2012;21:737-45. [Crossref] [PubMed]
- Care Quality Commissions Review of Deaths of NHS Patients. December2016. Available online: https://www.gov.uk/government/speeches/cqc-review-of-deaths-of-nhs-patients
- Hospital Standardised Mortality Ratio in Scotland. Health Improvement Scotland. June 2014.
- Hospital Standardised Mortality Ratio. April 2018 to March 2019. National Services Scotland. August 2019.
- Goodacre S, Campbell M, Carter A. What do hospital mortality rates tell us about quality of care? Emerg Med J 2015;32:244-7. [Crossref] [PubMed]
- Burns J, Airns G, Drummond L. NHS Lanarkshire Mortality Review Form. NHS Lanarkshire firstport. Available online: www.nhslanarkshire.scot.nhs.uk
- Hogan H, Zipfel R, Neuburger J, et al. Avoidability of hospital deaths and association with hospital-wide mortality ratios: retrospective case record review and regression analysis. BMJ 2015;351:h3239. [Crossref] [PubMed]
- Freemantle N, Richardson M, Wood J, et al. Weekend hospitalization and additional risk of death: an analysis of inpatient data. J R Soc Med 2012;105:74-84. [Crossref] [PubMed]
- Junior Doctors Contract. British Medical Association. Available online: www.bma.org.uk
Cite this article as: Mushtaq F, Mushtaq T, Amin N. Forty-eight-hour hospital mortality: an emergency department perspective studying the relationship between suboptimal care and mortality. J Emerg Crit Care Med 2021;5:14.



