
Cardiopulmonary resuscitation and risk of transmission of acute respiratory infections to rescuers: a systematic review snapshot
Introduction
High-quality cardiopulmonary resuscitation (CPR) and early defibrillation improve chance of survival during cardiac arrest (1,2). Current resuscitation guidelines highlight the importance of rescuer safety (1,2). In normal circumstances most cardiac arrest patients requiring CPR will not have an acute respiratory infection that has a high risk of transmission to health care workers (HCWs), including providers of CPR (3). However, the delivery of CPR to a patient infected with COVID-19 may place HCWs at risk.
The coronavirus (COVID-19) pandemic has highlighted the need for reassessment of acute respiratory infection transmission risks for healthcare providers (4,5). More importantly, the reassessment of those lifesaving interventions performed when attempting treatment of cardiac arrest that may generate aerosols that remain infectious when suspended in air, increasing the risk of infectious transmission (6-9).
This systematic review snapshot summarizes estimates for pooled data on the basis of the available evidence evaluating procedures that might generate aerosols or droplets and the risk of transmission of acute respiratory infections to HCWs. Unfortunately, most of the data comes from the fast severe acute respiratory syndrome coronavirus (SARS-CoV) epidemic in 2002–2003 (10).
Aims and objective
The aim of this systematic review snapshot was to identify and summarize in the form of a clinical synopsis the literature surrounding the potential risk of infection transmission associated with key interventions performed in the context of cardiac arrest.
Methods
Data sources
Data sources were PubMed, EMBASE, MEDLINE, CINAHL, the Cochrane Library, Index Medicus for South East Asia, LILACS, Indian Medlars, EuroScan, University of York CRD databases (01/01/1990 to 10/22/2010), Google and other Internet search engines, references of relevant articles and previously published literature, and, through contacts, experts in the field for article recommendations or unpublished work.
Study selection
Randomized controlled trials, non-randomized studies, systematic reviews, and meta-analyses. The study population involved HCWs caring for patients with acute respiratory infections undergoing aerosols generated procedures (AGPs) and the researches evaluated the risk of transmission of acute respiratory infections from patients to HCWs. Their predefined outcome of interest was the risk of transmission of acute respiratory infections from patients to HCWs. Exclusion criteria were not reported.
Data extraction and synthesis
One investigator extracted data after independently assessing each study for methodological quality. Relevant data was verified by a second investigator using the predesigned data extraction form to capture the study characteristics and the outcomes of interest. Effect sizes were reported as odds ratio (OR) and its 95% confidence interval (CI). The authors used random-effects modeling for the meta-analyses and heterogeneity was assess by using the I2 statistics. Where statistical heterogeneity was found, sensitivity analysis on treatment effect was conducted. Publication bias was not assessed. The authors calculated summary estimates of procedures that might promote the generation of aerosols or droplets and their association with the risk of transmission of acute respiratory infections from patients to HCWs.
Results
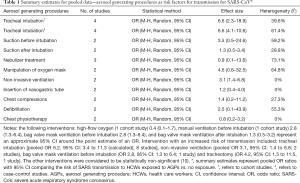
The authors identified 1,862 potential studies, of which 10 met the inclusion criteria (3,075 HCWs). No randomized controlled trials were identified. There were five non-randomized cohort studies and five retrospective cohort studies. All studies investigated the risk factors for transmission of SARS-CoV from patients to HCWs during the 2002–2003 SARS outbreaks. Most of the included studies were each conducted at single centers. Five studies were carried out in China, four in Canada, and one in Singapore. The majority of the studies evaluated whether HCWs had proper infection control training or wore personal protective equipment (PPE) while caring for patients with SARS. There was high heterogeneity across predictors of interest (range, 0% to 73.1%). Confounding was a universal source of bias across all studies included studies, given the observational nature of the evidence. The quality of the evidence was rated very low according to GRADE (11). Table 1 shows the risk of SARS transmission to HCWs exposed to AGPs compared to no exposure.
Full table
Commentary
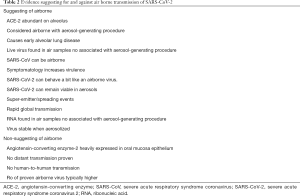
During the global spread of SARS (12,13), a great deal was discovered about the illness and the SARS-associated coronavirus (14,15). Studies from the SARS-CoV epidemic suggest that some procedures performed during CPR, including chest compressions, defibrillation, bag valve mask ventilation, or endotracheal intubation are potentially capable of generating aerosols associated with increased risk of SARS transmission to HCWs or were a risk factor that increase infection for transmission, with the most consistent association across multiple studies of increased risk for transmission identified with endotracheal intubation (10). The aim of this systematic review snapshot is to present a clinical synopsis of the risk of transmission of SARS-CoV infection to HCWs exposed to patients undergoing AGPs compared with the risk of transmission to HCWs caring for patients not undergoing AGPs. This review also attempts to highlight the lack of adequate studies regarding the topic and SARS-CoV-2. Although no direct clinical implications are immediately available this definitely is a necessary first step in summarizing the data or the lack of till date. At the same time this review does not attempt to question whether this deadly, novel, yet closely related coronavirus is airborne, as this remains strongly debated and is, presently, unclear. Table 2 outlines the existing arguments suggesting for and against air borne transmission of SARS-CoV-2.
Full table
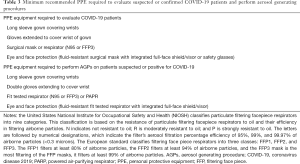
Respiratory infections in which the pathogens can cause diseases such as influenza, SARS, and COVID-19 have high morbidity and mortality. On February 11, 2020, the World Health Organization (WHO) announced the newly identified coronavirus that causes COVID-19, which has been called SARS-CoV-2. As of February 5, 2021, a total of 105,243,379 cases, including 2,294,180 deaths, have been reported in at least 192 countries/regions (16). The WHO has categorized CPR as an aerosol generating procedure (AGP) (4,5). However, to date little is known about SARS-CoV-2 and the risk of transmission to HCWs, including the risk of AGPs performed by providers during CPR. PPE protocols have been proposed by several local, statewide, and international institutions, but these recommendations are based on very low-quality evidence. Table 3 outlines the minimum PPE needed to evaluate a patient with suspected or confirmed COVID-19 and to perform AGPs as recommended by the American Heart Association’ interim guidance for Basic and Advanced Life Support and the Centers for Disease Control and Prevention (8,17). Although SARS-CoV-2 is slightly different from the coronavirus that causes SARS, most of the data we have on the risk of acute respiratory infections transmission to HCWs exposed to AGPs, including lifesaving interventions such as CPR, comes from the SARS-CoV epidemic in 2002–2003 (10).
Full table
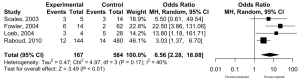
Unanswered questions persist and a significant research gap exists in this area. The debate on whether interventions performed during resuscitation should be considered AGPs remains unclear. Therefore, although there is almost no clear scientific evidence on which to base our decisions, during the current COVID-19 pandemic it is important that we understand the potential risk of transmission that can occur during resuscitation versus the known risk of resuscitation delays; many of these procedures, in particular endotracheal intubation, have been associated with transmission of acute respiratory infections to HCWs. Four cohort studies showed that HCWs performing or being exposed to a endotracheal intubation had a higher risk of disease transmission of SARS compared with the control group (unexposed HCWs). The study’s authors reported a pooled OR for this outcome of 6.6 with a 95% CI of 2.3 to 18.9 (P<0.0005; 4 cohort studies; 584 controls and 167 cases; very low-quality evidence) (Figure 1) (10). Four case-control studies identified that endotracheal intubation was a significant risk factor for transmission of SARS to HCWs compared with the control group (unexposed HCWs). The study’s authors reported a pooled OR for this outcome of 6.6 with 95% CI of 4.1 to 10.6 (P<0.0001; 4 case control studies; 1,454 controls and 259 cases; very low-quality evidence) (Table 1) (10). However, the overall certainty of the evidence was very low and at high risk of bias.
It is noteworthy that some of these interventions were performed with very sick patients, which is an important potential factor for confounding and a stronger predictor of HCWs contracting the infection than the procedure itself. Critically ill patients should be managed with the highest precautions; full enhanced PPE is recommended when managing patients during resuscitation especially during the COVID-19 pandemic to reduce the risk of SARS-CoV-2 transmission from patients with an unknown or known COVID-19 status. This review also serves as an effort to present some of the most common procedures performed during CPR that are potentially capable of generating aerosols which could increase the risk of transmission of acute respiratory infections to HCWs and to announce rescuer workers that we are still in the dark about the risks of infection transmission from COVID-19 during the aforementioned procedures and thus open the gates for studies to be initiated as we did not find any direct evidence that lifesaving procedures performed during CPR either are or are not associated with transmission of infection. Even though the basic reproductive rate (R0) for SARS-CoV-2 seems to be comparable to SARS-CoV 2.5 (range, 1.8–3.6) vs. 2.0–3.0 (18), we cannot conclude the risk of transmission of COVID-19 is same with SARS-CoV. It is very critical issue, and it might too early to think that this deadly, novel, yet closely related coronavirus imposed the same or higher risk of transmission of SARS.
Research priorities
- While performing endotracheal intubation is there evidence of increased risk of acute respiratory infection transmission to HCWs?
- While performing endotracheal intubation is there evidence that this procedure can be done safely without full enhanced PPE?
Acknowledgments
This is a clinical synopsis that used published aggregate data as opposed to individual subject data. The source for this systematic review snapshot is: Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol Generating Procedures and Risk of Transmission of Acute Respiratory Infections to Healthcare Workers: A Systematic Review. PLoS One 2012;7:e35797.
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-158). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132:S444-64. Erratum in: Circulation 2015 Dec 15;132(24):e385. doi: 10.1161/CIR.0000000000000347. [Crossref] [PubMed]
- Soar J, Nolan JP, Böttiger BW, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation 2015;95:100-47. [Crossref] [PubMed]
- Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019;139:e56-e528. Erratum in: Circulation 2020 Jan 14;141(2):e33. doi: 10.1161/CIR.0000000000000746. Epub 2020 Jan 13. [Crossref] [PubMed]
- World Health Organization. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. Available online: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations (accessed 27.07.20).
- World Health Organization. Infection prevention and control during health care when COVID-19 is suspected: interim guidance – 19 March 2020. Available online: https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125 (accessed 27.07.20).
- World Health Organization. Infection prevention and control of epidemic- and pandemic-parone acute respiratory infaections in health care: WHO guidelines. Geneva: World Health Organization, 2020.
- Couper K, Taylor-Phillips S, Grove A, et al. COVID-19 in cardiac arrest and infection risk to rescuers: A systematic review. Resuscitation 2020;151:59-66. [Crossref] [PubMed]
- Edelson DP, Sasson C, Chan PS, et al. Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID-19: From the Emergency Cardiovascular Care Committee and Get With The Guidelines-Resuscitation Adult and Pediatric Task Forces of the American Heart Association. Circulation 2020;141:e933-43. [Crossref] [PubMed]
- Nolan JP, Monsieurs KG, Bossaert L, et al. European Resuscitation Council COVID-19 guidelines executive summary. Resuscitation 2020;153:45-55. [Crossref] [PubMed]
- Tran K, Cimon K, Severn M, et al. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One 2012;7:e35797 [Crossref] [PubMed]
- Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383-94. [Crossref] [PubMed]
- Poutanen SM, Low DE, Henry B, et al. Identification of severe acute respiratory syndrome in Canada. N Engl J Med 2003;348:1995-2005. [Crossref] [PubMed]
- Booth CM, Matukas LM, Tomlinson GA, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA 2003;289:2801-9. Erratum in: JAMA 2003 Jul 16;290(3):334. [Crossref] [PubMed]
- Ksiazek TG, Erdman D, Goldsmith CS, et al. A novel coronavirus associated with severe acute respiratory syn- drome. N Engl J Med 2003;348:1953-66. [Crossref] [PubMed]
- Drosten C, Günther S, Preiser W, et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med 2003;348:1967-76. [Crossref] [PubMed]
- Johns Hopkins University CSSE. Wuhan coronavirus (2019-nCoV) global cases Available online: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 (accessed 02.05.21).
- CDC Recommendations on Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
- Petersen E, Koopmans M, Go U, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis 2020;20:e238-44. [Crossref] [PubMed]
Cite this article as: Miraglia D. Cardiopulmonary resuscitation and risk of transmission of acute respiratory infections to rescuers: a systematic review snapshot. J Emerg Crit Care Med 2021;5:17.


