A case report of rescue in extremis of mediastinal impalement: more fear than harm
Introduction
The cases of mediastinal impalement are infrequently encountered and rarely report in literature because the majority of these patients die in pre-hospital care. More than 90% of thoracic great vessel injuries are due to penetrating trauma and includes the aorta (ascending, arch and its branches, and descending aorta), the pulmonary vessels, the intrathoracic vena cava, and the innominate and azygos veins (1). Victims who are physiologically unstable after the injury to any of mediastinal compartments must be dealt with by the surgeons available without delay (2). Surviving patients with hemodynamic stability require a well-defined and codified management strategy if local technical expertise is limited (2). Based on this observation, we describe an unexpected non-fatal of penetrating intra-mediastinal injury and via a literature review, the tricks and tips of surgical management are discussed in a stable patient. We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jeccm-20-116).
Case presentation
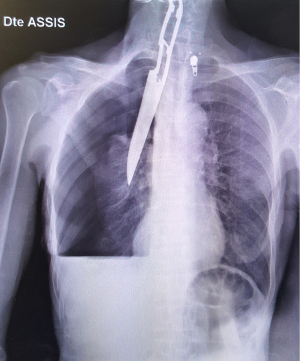
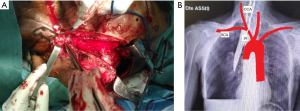
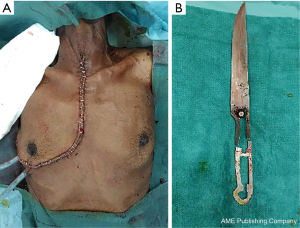
A 58-year-old female with no medical or medication-use history was presented to the emergency department of the University Hospital of Antsiranana (Northern of Madagascar 1,118 km away by road from Antananarivo the capital versus 759 km as the crow flies =50 min by aircraft) with history of homicide in the context of family vindictiveness. She was found by emergency physicians with a knife rammed into her cervical-thoracic region. The knife entered through jugular/suprasternal notch. On admission, the patient was fully conscious with the Glasgow Coma Scale was 14/15 and respiratory function was not compromised. All vital signs were normal with no neurologic deficits and stable (blood pressure 110/80 mmHg and heart rate 102 bpm). Clinical examination revealed no active bleeding at the entry sites and no signs of subcutaneous emphysema. Examination of the chest revealed no exit site for the stab. She was started on prophylactic antibiotics and tetanus antitoxin before surgery. Standard laboratory tests showed an elevation of white blood cell count to 14,000/mm3 (4,500 to 11,000 per mm3) and there was no significant haemoglobin reduction. The Focused Assessment Sonogram for Trauma (FAST) suspected right haemothorax and pneumothorax. Chest radiograph of the patient demonstrated a knife, penetrating the mediastinum and through in right pleura cavity leading a pneumo-haemothorax (Figure 1). No widening of the cardiac silhouette was established. CT scan was unavailable as an emergency. Due to the absence of a thoracic surgeon on the site, a thoracic surgeon from the capital was flying to Antsiranana to operate the patient in an emergency. Twenty-four hours after being admitted, the patient was immediately transferred to the emergency operating room for removal of the impaled objects under direct vision and injury control. Initially, the median sternotomy was performed immediately. Exploration of the mediastinal space revealed that the innominate artery passed through the hole in the tail of the knife, which was already broken at the lower edge
Discussion
Penetrating transmediastinal injury also called impalement mediastinal injury is defined as evidence of a single missile entry and exit on opposite sides of the thorax, missile entry and missile retention on opposite sides of the thorax, and missile entry on one side of the thorax with missile retention in the mediastinum as in our observation (1-3). The clinical presentation of mediastinal vessel injury following penetrating trauma may be acute or subacute as seen in our case. It depends on multiple factors, both extrinsic (mechanism, type of cutting object, type of firearm) and the severity of the injury to the intra-mediastinal vessels involved. This often presents a diagnostic and operative challenge to the thoracic surgeon and a decision to undergo an operation must be made with full knowledge of the facts. The surgical therapeutic approach must be adapted to the clinical status of the patient particularly patient’s hemodynamic status. Patients who are stable after adequate resuscitation may benefit from rapid chest X-ray imaging, computed tomographic angiography, and endovascular treatment by angiographic catheterization (1). A repeated examination with FAST echo is important to avoid missing or a possible aggravation of an unrecognized initial lesion. According to Guivarch et al. (4), CT scanning is definitely relevant in cases of thoracoabdominal and supraclavicular injuries and abnormal chest radiographs, as new lesions are frequently observed in these circumstances and have a significant impact on patient management. With the evolution of modern diagnostic and radiologic investigations including combined arteriography, esophagoscopy, bronchoscopy, and echocardiography help to decrease unnecessary explorations in hemodynamically stable patients. Historically, mandatory good operative exposure was the practice of any suspicion of intramediastinal vascular injury (1). VATS remains controversial especially in cases of suspected cardiac or major vessel injury (5-7). Chest drainage can be a diagnostic as well as a therapeutic procedure. It will be used to evacuate the intrapleural effusion in order to quantify blood, detect massive air leaks, and establish an operative indication for an invasive thoracotomy (6). Due to the limited diagnostic resources (scanner and VATS not available in the institution of Antsiranana), a sternotomy associated with a lateral thoracotomy (hemi-clamshell incision) allowed us to carry out a precise lesion assessment and control of pleuro-pulmonary haemorrhagic lesions. In this present case, there were no intramediastinal lesions. In our case, the operative indication was not debated despite the hemodynamic stability as the removal of the intra-mediastinal object without visual control will be fatal for our patient. The spared mediastinum organs and the associated well-tolerated haemopneumothorax would probably explain the haemodynamic and respiratory stability of our patient. Our attitude enabled us to safely remove the stab wound. This principle is adopted by several authors in the literature (7-9). In literature, penetrating injuries to the mediastinum usually have a high probability of injury to the vascular and other vital structures (1). Our patient’s survival before surgery is attributed to the non-existence of a fatal intramediastinal injury.
Conclusions
Removal of objects embedded in the chest may result in serious haemorrhage, hemodynamic damage and rapid cardiac arrest of victim and requiring a thorough study of each case planning and delicate process. This is why impaled penetrating objects impaled in the chest are systematically and mandatorily removed in the operating room under optimal conditions under direct visual and general anaesthesia. Early diagnosis and surgery can save patients who would otherwise be lost. In a country such as Madagascar where resources are generally extremely limited, all general surgeons should be trained in the management of this type of trauma to prevent further damage to the patient due to a delay in care in the absence or unavailability of the thoracic surgeon on-site.
Patient perspective
Even if the management of her illness was difficult, the patient was grateful to the entire medical team.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jeccm-20-116
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-116). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participant were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and any accompanying imagines.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Navsaria PH, Chowdhury S, Nicol AJ, et al. Penetrating trauma to the mediastinal vessels: a taxing injury. Curr Trauma Rep 2016;2:1-10. [Crossref]
- Yilmaz TH, Evers T, Sussman M, et al. Operating on penetrating trauma to the mediastinal vessels. Scand J Surg 2014;103:167-74. [Crossref] [PubMed]
- Gunn ML, Clark RT, Sadro CT, et al. Current concepts in imaging evaluation of penetrating transmediastinal injury. Radiographics 2014;34:1824-41. [Crossref] [PubMed]
- Guivarch E, Augustin P, Desmard M, et al. Stratégie de prise en charge des plaies thoraciques par arme blanche dans un déchoquage: Une série consécutive de 153 patients. Mémoire de DES: anesthésie et réanimation. Paris: Académie de paris, 2013:1.
- Tang X, Chen H, Chen C, et al. A case report of a polytrauma patient with penetrating iron rods in thorax and head. Medicine (Baltimore) 2018;97:e12376. [Crossref] [PubMed]
- Dalavi SB, Gurav PD, Sharad SS. Penetrating chest injury: a miraculous life salvage. Med J DY Patil Univ 2013;6:440. [Crossref]
- Novakov IP. Thoracic stab wound: a curious case report. Clin Surg 2018;3:2183.
- Mercier PP, de REIMS CHU, Harouna PO. Annales de l’Université Abdou Moumouni de Niamey, Tome XIV, 2013 Série A: Sciences exactes, naturelles, agronomiques et de la santé Comité de lecture. In: Annales de l’Université Abdou Moumouni de Niamey. 2013.
- Etoundi PO, Bob’oyono JM, Ela AA, et al. Plaie pénétrante thoracique par jet de lance. HealthSci Dis 2014;15:1-3.
Cite this article as: Razafimanjato NNM, Andrianony A, Rabemazava AZLA, Rakotovao HJL. A case report of rescue in extremis of mediastinal impalement: more fear than harm. J Emerg Crit Care Med 2022;6:8.