
Pheochromocytoma crisis treated with veno-arterial extracorporeal membrane oxygenation and urgent adrenalectomy—case report
Introduction
Pheochromocytoma is usually diagnosed as an incidental finding on abdominal imaging, or as part of secondary hypertension work-up, with or without suspicious symptoms. Treatment is surgical resection, however appropriate medical preparation is necessary in order to prevent perioperative cardiovascular complications.
It is on this background, that we report a case of cardiogenic shock requiring veno-arterial extracorporeal membrane oxygenation (VA-ECMO) support, unveiling a diagnosis of pheochromocytoma, and treated with urgent adrenalectomy.
We present the following case in accordance with the CARE reporting checklist (available at https://dx.doi.org/10.21037/jeccm-21-32).
Case presentation
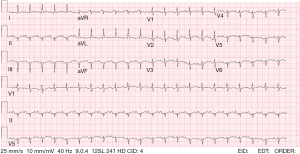
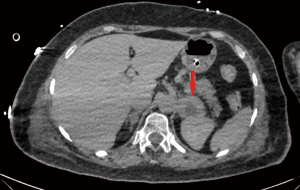
A 61-year-old woman presents to the Emergency Department (ED) with respiratory failure. She is a highly functional, physically active woman, and her medical history includes complicated migraine and past smoking. Earlier that day she underwent a face-lift surgery in a private medical facility. Her intraoperative course included highly labile blood pressure (BP) ranging between 180 and 60 systolic as well as heart rate (HR) ranging between 160 and 30. The surgery was shortened to the minimally necessary and the patients was transferred extubated to the post-anesthesia care unit where she gradually developed hypoxemic respiratory failure while the hemodynamic lability continued, leading to her transfer to our ED. In the ED her temperature was 38.5 °C, HR 145 beats/min, BP 96/72 mmHg, and oxygen saturation 72% on ambient air. Her skin was cold and mottled, jugular venous pulse could not be evaluated due to postoperative neck edema. Auscultation yielded remote and rapid heart sounds and scattered pulmonary crackles. Her white blood cell count was 21.8×109/L, creatinine 1.3 mg/dL, arterial pH 7.11, lactate 6.8 mmol/L, troponin I 6,335 ng/L, B-type natriuretic peptide 1,022 pg/mL, and C-reactive protein 19.1 mg/L. An electrocardiogram showed sinus tachycardia, left axis deviation, mild widespread up-sloping ST-segment elevation and poor R wave progression (Figure 1).Chest X-ray showed bilateral alveolar infiltrates with air bronchogram (Figure 2). An emergent transthoracic echocardiogram demonstrated severe left ventricular (LV) systolic dysfunction, with somewhat sparing of the base, and akinesis of the remaining walls including the apex (Video S1). The combination of acute heart and respiratory failure along with fever, leukocytosis and bilateral alveolar infiltrates raised suspicion for COVID-19, and the patient underwent chest CT that demonstrated bilateral consolidations with crazy paving pattern, as well as a round lesion with a hypodense core in the left adrenal gland, measuring 4.2 cm in diameter (Figure 3).
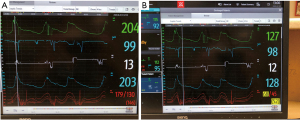
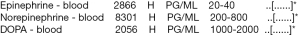
The patient rapidly decompensated and received mechanical ventilation and vasopressor support and was admitted to the ICU for the management of cardiogenic shock. Within 2 hours from admission, her status further deteriorated to severe hypoxemia, refractory hypotension and bradycardia requiring CPR and 1mg of Epinephrine. Peripheral veno-arterial extracorporeal membrane oxygenation (VA-ECMO) was urgently initiated (Video S2), resulting in rapid stabilization of HR, MAP, SaO2%, normalization of lactate levels and pH, and restoration of normal urinary output. At this point, given the pattern of global LV dysfunction, absence of marked ST elevations or Q-waves on ECG, absence of angina complaints while experiencing hypertension surge during surgery, the presence of fever and lung infiltrates, and relatively low levels of Troponin I, the diagnosis of acute MI seemed unlikely and no coronary angiography was undertaken. A provisional diagnosis of Takotsubo versus myocarditis was suspected. The patient was treated with antibiotics, dobutamine, epinephrine, norepinephrine, and stress dose hydrocortisone (200 mg/d), following by addition of Levosimendan. Investigation of bacterial and viral agents was negative, including for SARS-CoV2. During the following days LV function quickly recovered (Video S3), allowing successful weaning from ECMO support on day 5,however recurrent episodes of marked hypertension and tachycardia lasting 5–10 minutes occurred, followed by a sudden drop in BP. An example of such cyclic events is shown in Figure 4. The distinct pattern of these events, combined with the incidental finding of a left adrenal mass raised a high suspicion of pheochromocytoma and indeed the family describes recurrent events of palpitation and flushing followed by dizziness and near syncope. Blood levels of catecholamine confirmed extremely high levels of Epinephrine (2,866 µg/mL) and Norepinephrine (8,301 µg/mL), 71.65 and 10.37 times the upper limit of normal, respectively (Figure 5).
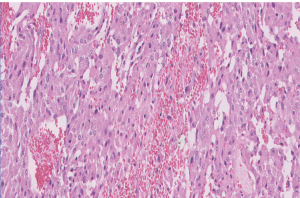
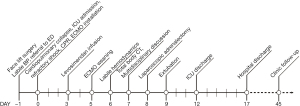
Abdominal CT was without evidence of multinodular or metastatic disease. Following a multidisciplinary discussion that included intensivists, endocrinologists, anesthetists and surgeons, urgent laparoscopic left adrenalectomy was safely performed on day 8, yielding a 4.0 cm × 3.0 cm × 5.0 cmtumor that was confined within the adrenal capsule and had extensive hemorrhagic features (Figure 6). Pathologic analysis confirmed the diagnosis of pheochromocytoma (Figure 7). The patient was extubated on day 9 and discharged from the ICU and the hospital at days 11 and 17 respectively, with a diagnosis of pheochromocytoma crisis inducing cardiogenic shock. She did not require further medical therapy and remained clinically stable and asymptomatic on follow-up at 4, and 12 weeks. A timeline of key events during course of illness, and the anesthetic chart during adrenalectomy are illustrated in Figure 8 and Figure 9 respectively.

All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Patient’s perspective
My name is ML, I am 61 at the time of the events. I am a mother of 6 and a grandmother if 12. I am a very active and dominant woman. I went to the plastic surgery with the thought of finally doing something for myself, since I always take care of everybody and find myself at the bottom of my priorities. My only prior symptom was heat waves, occasionally accompanied by a feeling of my heart beating super strong and my hands shaking, a feeling of chest pressure and profuse sweating. Once I performed an ECG that was normal. I figured it was menopausal symptoms.
I went to the procedure with a good and confident feeling. I remember meeting the anesthesiologist in the morning, and the next memory I have is waking up in the intensive care unit. Only days after I woke up I realized how long I was in the hospital for and what my family has gone through. I remember absolutely nothing from the cosmetic surgery until after the adrenalectomy.
Eventually I was discharged home and made a complete recovery thanks to a home-rehabilitation program and the help and support of my wonderful family.
Discussion
We present a case of pheochromocytoma induced cardiogenic shock, treated with VA-ECMO and urgent adrenalectomy. ECMO has become a widespread tool in cases of cardiopulmonary collapse, with best results in cases of rapidly reversible etiologies such as myocarditis or Takotsubo syndrome (1-4). Pheochromocytoma crisis is a feared and potentially lethal complication of pheochromocytoma (5,6), that can occur spontaneously or be precipitated by manipulation of the tumor, trauma, certain medications (corticosteroids, β-blockers, metoclopramide, and anesthetic agents), or stress from nonadrenal surgery. The use of ECMO for acute heart failure due to pheochromocytoma crisis has been described in the past (7-9). As in many other medical scenarios, treating the primary etiology is key to recovery. However, in the case of pheochromocytoma crisis, the wish to achieve proper alpha and beta blockade prior to surgical adrenalectomy, as recommended for elective surgery (10), needs to be weighed against the benefits and risks of urgent adrenalectomy. The debate whether pheochromocytoma crisis is a surgical emergency remains unsettled.
NANETS consensus guidelines recommend pre-operative medical treatment to block the effects of catecholamines for at least 10–14 days before surgery (11).Scholten et al. reported high surgical morbidity and mortality for emergent and urgent adrenalectomy in comparison with elective surgery following medical treatment, however patients in the first group required more ICU admissions and hemodynamic support, and had larger tumors (12). In a case series and literature review by Hekimian et al., most patients underwent safe elective adrenalectomy after hemodynamic stabilization and proper medical preparation (9).
On the other hand, already in 1988, Newell et al. reported that the only survivors in a series of patients with pheochromocytoma crisis, were the two patients that underwent urgent adrenalectomy (13). Later on, in 2017, Sauneuf et al. published a 16-year French-multicenter retrospective of 34 patients with pheochromocytoma crisis in which all early-operated patients (5 out of 34 patients, 14.7%) were discharged alive from the hospital, including 2 patients operated while on ECMO support, while overall 90-day mortality was 27% (9 of 34) (14).
In summary, we present a case of pheochromocytoma crisis, requiring invasive hemodynamic support, in which urgent adrenalectomy was safely performed without prior medical stabilization as means of immediate control of the offending source. Further prospective trials are necessary in order to evaluate whether immediate surgical intervention is safe and beneficial in such extreme cases.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://dx.doi.org/10.21037/jeccm-21-32
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/jeccm-21-32). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Combes A, Leprince P, Luyt CE, et al. Outcomes and long-term quality-of-life of patients supported by extracorporeal membrane oxygenation for refractory cardiogenic shock. Crit Care Med 2008;36:1404-11. [Crossref] [PubMed]
- Thiagarajan RR, Barbaro RP, Rycus PT, et al. Extracorporeal Life Support Organization Registry International Report 2016. ASAIO J 2017;63:60-7. [Crossref] [PubMed]
- Keebler ME, Haddad EV, Choi CW, et al. Venoarterial Extracorporeal Membrane Oxygenation in Cardiogenic Shock. JACC Heart Fail 2018;6:503-16. [Crossref] [PubMed]
- Takayama H, Truby L, Koekort M, et al. Clinical outcome of mechanical circulatory support for refractory cardiogenic shock in the current era. J Heart Lung Transplant 2013;32:106-11. [Crossref] [PubMed]
- Riester A, Weismann D, Quinkler M, et al. Life-threatening events in patients with pheochromocytoma. Eur J Endocrinol 2015;173:757-64. [Crossref] [PubMed]
- Spangenberg T, Freker C, Niggemann C, et al. Differential diagnosis of a fulminant myocarditis: the pheochromocytoma crisis. Eur Heart J Acute Cardiovasc Care 2015;4:577-8. [Crossref] [PubMed]
- Flam B, Broomé M, Frenckner B, et al. Pheochromocytoma-Induced Inverted Takotsubo-Like Cardiomyopathy Leading to Cardiogenic Shock Successfully Treated With Extracorporeal Membrane Oxygenation. J Intensive Care Med 2015;30:365-72. [Crossref] [PubMed]
- Chao A, Wang CH, You HC, et al. Highlighting Indication of extracorporeal membrane oxygenation in endocrine emergencies. Sci Rep 2015;5:13361. [Crossref] [PubMed]
- Hekimian G, Kharcha F, Bréchot N, et al. Extracorporeal membrane oxygenation for pheochromocytoma-induced cardiogenic shock. Ann Intensive Care 2016;6:117. [Crossref] [PubMed]
- Naranjo J, Dodd S, Martin YN. Perioperative Management of Pheochromocytoma. J Cardiothorac Vasc Anesth 2017;31:1427-39. [Crossref] [PubMed]
- Chen H, Sippel RS, O'Dorisio MS, et al. The North American Neuroendocrine Tumor Society consensus guideline for the diagnosis and management of neuroendocrine tumors: pheochromocytoma, paraganglioma, and medullary thyroid cancer. Pancreas 2010;39:775-83. [Crossref] [PubMed]
- Scholten A, Cisco RM, Vriens MR, et al. Pheochromocytoma crisis is not a surgical emergency. J Clin Endocrinol Metab 2013;98:581-91. [Crossref] [PubMed]
- Newell KA, Prinz RA, Pickleman J, et al. Pheochromocytoma multisystem crisis. A surgical emergency. Arch Surg 1988;123:956-9. [Crossref] [PubMed]
- Sauneuf B, Chudeau N, Champigneulle B, et al. Pheochromocytoma Crisis in the ICU: A French Multicenter Cohort Study With Emphasis on Rescue Extracorporeal Membrane Oxygenation. Crit Care Med 2017;45:e657-e665. [Crossref] [PubMed]
Cite this article as: Lichter Y, Nini A, Szekely Y, Goder N, Schvartz R, Zac L, Topilsky Y, Vine J, Gal-Oz A. Pheochromocytoma crisis treated with veno-arterial extracorporeal membrane oxygenation and urgent adrenalectomy—case report. J Emerg Crit Care Med 2022;6:5.




