
Supports and barriers to implementing screening tools in public hospital emergency departments
Highlight box
Key findings
• In the emergency department (ED) screening tools (STs) are regularly promoted but due to environmental context, competing priorities, limited time and patient engagement, STs are not always utilised as designed.
What is known and what is new?
• STs are important eliciting potential conditions in a consistent manner for more standardized data collection and patient treatment. Research has shown that in other contexts barriers such as time, equipment, clinician and patient engagement can be barriers to their implementation.
• This manuscript adds the ED as a clinical context and speaks directly to the use of any ST rather than trialing a specific ST. The ED if often required to perform a range of STs in a busy and robust environment. It highlights the difficulty in completing all STs and how some ST designs do not feel relevant, or are not relevant to the patient in front of them. Further, some clinicians use a ST to confirm a suspicion rather than as a screen.
What is the implication, and what should change now?
• This has implications for clinical practice. STs may not be used which in turn may have implications for patient diagnosis and treatment. Or, if all STs are used this will limit a clinicians time to tend to other priorities. STs for the ED need to consider this environment, have clear organization guidelines and invest early in clinician motivation.
Introduction
Historically, screening tools (STs) have been used to test whether a person has a condition when there are no recognised symptoms and to reduce the impact of ill health (1). STs are an important measurement in providing clinicians with predictive values for at-risk populations (2). STs are a useful means of standardized criteria that promotes consistent data collection (3). For busy clinicians with limited training in complex diagnostics, adopting an ST is a crucial first step to ensure appropriate care (4). Further, being aware of how to screen effectively can improve a clinician’s ability to detect risks early (5). Barrera et al. (6) found that for healthcare clinicians, STs are useful for commencing healthcare conversations, triaging and facilitating clear documentation. A further benefit in the healthcare setting is that validated STs are low in cost to implement (7).
There are a number STs used in the ED to screen for various health, social, and safety concerns. Without identifying individual STs, these may include screening for stroke, substance use, family violence, falls, orientation, delirium, nutritional or mental health concerns to identify a few key areas. For the purpose of this study, an ST is differentiated from an initial assessment. The ST is used more broadly to identify any conditions, while an assessment is a more in-depth review of a presenting issue and known history or symptoms experienced.
There are, however, barriers to clinicians’ ability to complete or effectively use STs. These barriers include a clinician’s limited education and training about STs (8,9), poor understanding of what to do if a screen is positive (10), poor general resources such as access to equipment (6) and time constraints (11).
Emergency departments (EDs) are at the forefront for individuals requiring emergency treatment or presenting for less urgent health concerns (12) across all age ranges (13). It is a busy environment with increasing presentations (14,15) and a history of overcrowding (16,17). Increasingly, people are using EDs as a primary source of general healthcare and non-emergencies (18). With limited time, a high turnover of patients and a wide range of presentation types, the ED is often seen as the primary source for a range of STs to link patients with appropriate care.
There has been limited research into how ED staff utilise STs in a busy environment. This is an important clinical issue because EDs rely heavily on using STs to provide some direction toward diagnosis and treatment. If STs are not being used as designed, or not used at all due to workplace barriers, this will impact the management of a person in the ED. If there is a greater awareness of what facilitates proper use of STs in the ED, then better engagement and thus treatment is promoted.
This study aims to examine the extent to which STs are utilised in the ED and to identify any supports or barriers to their consistent implementation.
The study asks specifically:
- How are STs used in the ED?
- What are the barriers and supports that affect the use of STs in the ED?
Methods
The study location was in three separate EDs across the Melbourne-based Eastern Health network in Australia. Eastern Health is a public health service providing emergency, medical, surgical, rehabilitation, mental health and community-based services to all ages. The network covers the largest geographical area in the state of Victoria with a diverse community requiring different culture, age, socio-economics and healthcare requirements. The three EDs are a 24-hour service providing a wide range of emergency care to all ages that could include resusutative care, mental health crisis support and a wide range of emergency and accident care.
This is a mixed-methods study utilising the benefits of quantitative data to examine for trends and a thematic analysis of qualitative data to give these trends a context (19). Participants were ED clinicians who were invited to participate opportunistically (depending on availability and department need) during shifts. To be eligible the clinician was required to be employed either as nursing, allied health, or medically trained and based primarily in the ED. Clinicians had to have been working in the ED at least one year as a registered clinician. The researcher was based in the tearoom with hardcopy surveys placed on tables to promote convenience sampling. If these were completed they were immediately filed in an envelope and stored securely. As with ethics protocols participants were voluntary and could withdraw from completing the survey at any time, with their responses kept anonymous.
The survey had 11 questions with six being quantitative and the remaining qualitative. The quantitative section asked people to grade the usefulness or importance of a STs with the specific questions outlined in the results analysis. In summary, the survey asked participants to consider, within the ED context, the general usefulness of STs, the amount of STs they are asked to complete, the length of STs, how often they use STs, how they are prompted to use STs, benefits of STs, barriers to STs, enablers to use STs, recommendations for ST design and any useful STs used in the ED.
A systematic analysis approach was taken by the author to search for common themes (20) within the qualitative data provided by participants. The general themes were divided into ‘barriers’ and ‘enablers’. Within these themes further coding provided context to these enablers. These were further coded into areas the participant identified. These included; access to equipment, being time poor, patient engagement, attitudes towards STs, or having other priorities. Saturation was determined when consistent themes were occurring repeatedly (21) and each of the three EDs had a similar sample size. These themes are more specifically described in the proceeding results section.
Ethical considerations
The survey was brief to minimise clinical load interference and was approved by the hospital ethics committee (#LR20056) and the ED director. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent is implied after an explanatory letter of invitation to participate was provided and survey completion by all individual participants.
Results
A total of 61 participants completed the survey, with a close-to-even spread of participants across each of the three EDs. Of the participants, 6 were allied health professionals, 12 were medical practitioners, 4 were care coordinators (discharge planners) and 39 were nurses. All were working in the ED.
Part one of the results is the quantitative data with a 100% completion rate for this component of the survey. The general consensus was that STs had some value; however, not always. STs were considered always helpful by 5% of respondents, sometimes helpful for 52% of respondents, usually helpful for 41% and never helpful for 2%. The majority of respondents felt there were too many STs (57%); 35% stated there was the correct amount of STs and 8% felt more STs were needed in the ED. STs were generally considered to take too long to complete (64%); 34% stated the length of time to complete STs was suitable and 2% felt STs were generally too short to complete.
Participants were then asked how often they used the STs they were directed to complete, with the raw data results noted in Figure 1.
The nature of what prompts clinicians to use STs was examined. Most people regularly used an ST when they suspected there was a problem, rather than as a screen; 65% stated they often use STs in this manner. A further 8% stated they use STs solely when they suspect they are needed, while the remaining 27% stated they use them as part of an initial assessment or screen solely.
Part two of the results is qualitative, with each question yielding different levels of participation. The first question asked respondents to consider any barriers to using STs in the ED (N=53 at 86.9%). Responses were coded into themes, and some participants provided more than one response. The main responses were time barriers and the length of the ST. The full raw data results are presented in Figure 2.

One nurse responded by stating, ‘Some of them (STs) are so extensive and long that I avoid them. STs contain a lot of irrelevant and unnecessary tick boxes.’ An allied health professional stated, ‘A place to assess a person (is limited) and the loudness of the department. A cubicle that is available would be really helpful.’ A medical practitioner reported barriers, stating, ‘When they are not clinically indicated. The length of the ST and how well the patient can engage for that long.’ One nurse reported STs are ‘often not user friendly’, and another allied health clinician noted, ‘They are far too long to do in the ED, and I feel silly asking questions that are clearly not relevant.’ The theme of poor relevance did receive some traction, noting the ST often had little to do with the ED presentation and may have little interest to a patient experiencing a crisis or who is intoxicated.
Participants were then asked to consider what enablers there were to using STs, and there were 44 (72.1%) responses. Again, these were coded into themes with the raw data results in Figure 3.
One nurse responded that the best enabler to using an ST is ‘Short ones that are relevant to the complaint’. An allied health clinician stated, ‘Try to make it useful to the presentation and environment. Blanket “one fits all” STs never really help that much.’ One medical team member stated, ‘Proven effectiveness and relevance to the presenting issue’ was most important, while another nurse responded, ‘User-friendly tips, such as prompts or activities that populate automatically or add up scores automatically’, are good enablers. Finally, one nurse noted having a quiet shift was the best enabler, stating, ‘Not being busy, which almost never happens’.
Participants were then asked to make any recommendations for STs to be better used in the ED, and there were 31 (50.8%) responses. The themes are outlined below in raw data (Figure 4).
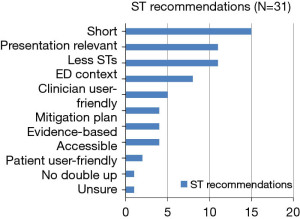
One care coordinator responded, ‘Just remember the ED is a busy place that is loud, and people are there for many reasons and probably distressed or would rather not be answering questions that are not helpful or engaging’. A medical practitioner stated, ‘Must be simple, verbally frugal, accessible at all times, instructive and have a definitive recommendation at the end’. Another nurse reported, ‘Consider that a person may not be able to respond for many reasons that can include how unwell they are physically or mentally’. One final nurse responded, ‘Make it short, accurate and relevant if you want it used in emergency’.
Next, respondents were asked to note any useful STs they use in the ED (N=19 at 31.1%). 52.6% noted the falls risk screen was useful, 21.1% stated the behaviours of concern (local screen) was useful, 16% reported the delirium ST was useful, and the same for harmful alcohol use.
Finally, participants were invited to make any open comments, and two comments (3.3% of participants) were made. One noted that senior medical practitioners’ exposure to STs was through junior doctors. One nurse responded that there were not enough mitigation plans, stating, ‘Just ticking a box doesn’t mean a clinician has done anything to address the identified risk. Which kind of makes it a redundant intervention’.
Discussion
It is well established that STs are an important resource, and many participants noted the value they see in the ED and use them regularly. Further, the ED is often a place where people seek regular health treatment outside of emergencies, which further justifies the importance of STs for people who may not have ready access to primary healthcare providers such as a general practitioner. This study found that STs that are brief, relevant, and can be used in the ED are all enablers to good clinician engagement. However, participants note that STs often do not consider the ED environment, which is a loud and busy atmosphere with the people being supported often in a level of crisis or focused on the presenting acute issue. Clinicians often use an ST to confirm a suspicion of an illness rather than to screen for it.
This study is reflective of some other findings. For example, Jacobsen (22) noted that the time and length to administer STs is a barrier to proper use. Kirk et al. (23) utilised the Theoretical Domains Framework to highlight that in an ED the environmental context, resources and, again, time were a barrier to completing STs. Poor access to equipment such as computers or technology limiting use of STs has also been replicated by Priaulx et al. (24). Finally, a patient’s ability to engage has also been shown to be a barrier at times in other studies, however they tend to note different literacy levels (25) or cultural backgrounds (6).
Loscalzo et al. (11) noted that to promote STs a clinician needs to have a clear understanding of the STs benefits and impact for patients, this can require a culture shift. While this may not resolve some of the environmental and workload issues the ED faces, it is a worthy method of increasing clinician engagement and promoting holistic care through screening. Further a clinician’s motivation will support the use of STs and addressing this early by ascertaining perceptions of the ST and clarifying the benefits of it early will enhance this motivation (26). At an organisational level, clear policy guidelines, expectations and practices are required to promote better use of STs (27).
There are some clinical risks if STs are not adapted well to the ED environment. This study has reflected that STs can be used in different ways or not at all depending on a range of personal, clinical and environmental factors. When it comes to clinical care this can result in missed or inconsistent diagnostic and treatment options putting the patient at risk. While lengthy STs can minimise attention to other patient care needs, especially if they are STs repeated throughout the shift across hundreds of daily ED presentations.
There are many STs that the ED staff are asked to complete, so STs need to be sharp and concise, relevant to the ED environment and include some form of escalation mitigation process. Otherwise, due to competing demands of the ED clinician, they may be used less, inappropriately or not at all.
Limitations
While the location of the study has some generalised use, the study cannot account for other rural or international regions. It is acknowledged that the survey was brief; however, a lengthy questionnaire is likely to reduce the ability of clinicians to participate. Participant motivation was not examined and would be a useful follow-up with consideration to the Theoretical Domains Framework of Change (23,28). The decision was made not to identify specific STs as it was felt this could be interpreted as a critique of specific STs rather than a clinician issue. To respect anonymity, sex/gender and length of time working in the ED was not sought to preserve anonymity. In the future it may be worth understanding if experienced clinicians use STs more than newer clinicians. Finally, there are some limitations in taking advantage of convenience sampling in this study. This is a relatively small sample size from one health network where participants were available making generalizability limited (29). Further, this is limited to the ED so comparisons with other areas would require caution.
Conclusions
STs are an integral part of healthcare and need to be effectively utilised in the ED context. However, the busy caseload, the physical environment of the ED, the perceived irrelevance of some STs to the presenting issue, the multiple STs to use, the patient’s ability to engage in a crisis, limited accessibility to the ST and the length of time some take to complete are barriers to the appropriate use of STs in the ED. Services developing STs to be used in the ED should consider these factors, while EDs could consider examining clinician motivation in using STs.
Acknowledgments
The author would like to thank Associate Professor Judy Hope and Dr. Peter Jordan for their support.
Funding: None.
Footnote
Data Sharing Statement: Available at https://jeccm.amegroups.com/article/view/10.21037/jeccm-24-42/dss
Peer Review File: Available at https://jeccm.amegroups.com/article/view/10.21037/jeccm-24-42/prf
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://jeccm.amegroups.com/article/view/10.21037/jeccm-24-42/coif). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the hospital ethics committee (#LR20056) and the ED director. Informed consent is implied after an explanatory letter of invitation to participate was provided and survey completion by all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Raffle AE, Gray JM. Screening: Evidence and practice. USA: Oxford University Press; 2019.
- Decoster L, Van Puyvelde K, Mohile S, et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: an update on SIOG recommendations†. Ann Oncol 2015;26:288-300. [Crossref] [PubMed]
- Giron NC, Cole MB, Nguyen KH. Use of and barriers to adopting standardized social risk screening tools in federally qualified health centers during the first year of the COVID-19 pandemic. Health Serv Res 2024;59:e14232. [Crossref] [PubMed]
- Ali GC, Ryan G, De Silva MJ. Validated Screening Tools for Common Mental Disorders in Low and Middle Income Countries: A Systematic Review. PLoS One 2016;11:e0156939. [Crossref] [PubMed]
- Vythilingum B, Field S, Kafaar Z, et al. Screening and pathways to maternal mental health care in a South African antenatal setting. Arch Womens Ment Health 2013;16:371-9. [Crossref] [PubMed]
- Barrera M, Alexander S, Shama W, et al. Perceived benefits of and barriers to psychosocial risk screening in pediatric oncology by health care providers. Pediatr Blood Cancer 2018;65:e27429. [Crossref] [PubMed]
- Pinto-Martin JA, Dunkle M, Earls M, et al. Developmental stages of developmental screening: steps to implementation of a successful program. Am J Public Health 2005;95:1928-32. [Crossref] [PubMed]
- Flaigle MC, Ascenzi J, Kudchadkar SR. Identifying Barriers to Delirium Screening and Prevention in the Pediatric ICU: Evaluation of PICU Staff Knowledge. J Pediatr Nurs 2016;31:81-4. [Crossref] [PubMed]
- Johnson M, Jackson R, Guillaume L, et al. Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: a systematic review of qualitative evidence. J Public Health (Oxf) 2011;33:412-21. [Crossref] [PubMed]
- Nygaard P, Aasland OG. Barriers to implementing screening and brief interventions in general practice: findings from a qualitative study in Norway. Alcohol Alcohol 2011;46:52-60. [Crossref] [PubMed]
- Loscalzo M, Clark KL, Holland J. Successful strategies for implementing biopsychosocial screening. Psychooncology 2011;20:455-62. [Crossref] [PubMed]
- Kellett J, Nickel CH. What are nonspecific complaints and what are their causes and outcomes? The common unknown unknowns of medicine. Eur J Intern Med 2018;47:e12-3. [Crossref] [PubMed]
- Freed GL, Gafforini S, Carson N. Age distribution of emergency department presentations in Victoria. Emerg Med Australas 2015;27:102-7. [Crossref] [PubMed]
- Wardrop R, Crilly J, Ranse J, et al. Vulnerability: A concept synthesis and its application to the Emergency Department. Int Emerg Nurs 2021;54:100936. [Crossref] [PubMed]
- Morley C, Stankovich J, Peterson G, et al. Planning for the future: Emergency department presentation patterns in Tasmania, Australia. Int Emerg Nurs 2018;38:34-40. [Crossref] [PubMed]
- Savioli G, Ceresa IF, Gri N, et al. Emergency Department Overcrowding: Understanding the Factors to Find Corresponding Solutions. J Pers Med 2022;12:279. [Crossref] [PubMed]
- Di Somma S, Paladino L, Vaughan L, et al. Overcrowding in emergency department: an international issue. Intern Emerg Med 2015;10:171-5. [Crossref] [PubMed]
- O'Cathain A, Connell J, Long J, et al. 'Clinically unnecessary' use of emergency and urgent care: A realist review of patients' decision making. Health Expect 2020;23:19-40. [Crossref] [PubMed]
- Palinkas LA, Horwitz SM, Green CA, et al. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm Policy Ment Health 2015;42:533-44. [Crossref] [PubMed]
- Neuendorf KA. Content analysis and thematic analysis. In Advanced research methods for applied psychology. Routledge 2018:211-23.
- Fusch PI, Ness LR. Are we there yet? Data saturation in qualitative research. The Qualitative Report 2015;20:1408-16. [Crossref]
- Jacobsen PB. Screening for psychological distress in cancer patients: challenges and opportunities. J Clin Oncol 2007;25:4526-7. [Crossref] [PubMed]
- Kirk JW, Sivertsen DM, Petersen J, et al. Barriers and facilitators for implementing a new screening tool in an emergency department: A qualitative study applying the Theoretical Domains Framework. J Clin Nurs 2016;25:2786-97. [Crossref] [PubMed]
- Priaulx J, de Koning HJ, de Kok IMCM, et al. Identifying the barriers to effective breast, cervical and colorectal cancer screening in thirty one European countries using the Barriers to Effective Screening Tool (BEST). Health Policy 2018;122:1190-7. [Crossref] [PubMed]
- MacWilliams K, Curran J, Racek J, et al. Barriers and Facilitators to Implementing the HEADS-ED: A Rapid Screening Tool for Pediatric Patients in Emergency Departments. Pediatr Emerg Care 2017;33:774-80. [Crossref] [PubMed]
- Petersen HV, Sivertsen DM, Jørgensen LM, et al. From expected to actual barriers and facilitators when implementing a new screening tool: A qualitative study applying the Theoretical Domains Framework. J Clin Nurs 2023;32:2867-79. [Crossref] [PubMed]
- Lim SH, Ang SY, Abu Bakar Aloweni FB, et al. An integrative review on screening for frailty in acute care: Accuracy, barriers to implementation and adoption strategies. Geriatr Nurs 2019;40:603-13. [Crossref] [PubMed]
- Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7:37. [Crossref] [PubMed]
- Emerson RW. Convenience sampling revisited: Embracing its limitations through thoughtful study design. Journal of Visual Impairment & Blindness 2021;115:76-7. [Crossref]
Cite this article as: Donley E. Supports and barriers to implementing screening tools in public hospital emergency departments. J Emerg Crit Care Med 2024;8:19.




